Adult Care Transition Guide for Childhood Cancer Survivors

You might feel nervous when you think about moving from pediatric to adult care. Early planning helps you feel more confident and supported. Pediatric teams guide you and your family, making sure you learn to speak up for your health needs. Survivorship care plans, or SCPs, boost survival rates and help you stay healthy as you grow. Check out the table below to see how SCPs make a difference in The Transition to Adult Care for Childhood Cancer Survivors:
Description | Importance |
|---|---|
SCPs improve survival rates | Shows how planning early helps you live longer |
SCPs are key tools | Helps you get better care, not just paperwork |
Large study links SCPs to survival | Proves planning matters for your future |
CDC supports SCPs for transition | Makes sure you get the right care as you move to adult services |
You and your family can trust that a well-managed transition brings real benefits for your future health.
Key Takeaways
Start planning for your transition to adult care around age 12. Early preparation builds confidence and helps you learn important health skills.
Create a survivorship care plan to track your medical history and health needs. This plan improves your care and helps you communicate with new doctors.
Develop self-advocacy skills by practicing how to ask questions and express your health concerns. This empowers you to take charge of your care.
Choose adult care providers who understand your history and can coordinate with your previous doctors. Good communication ensures you receive the best care.
Stay connected with your care team and keep a record of your health. Regular check-ins help you manage your health and prevent gaps in care.
Why the Transition to Adult Care for Childhood Cancer Survivors Matters
Long-Term Health Outcomes
You might wonder why The Transition to Adult Care for Childhood Cancer Survivors is such a big deal. Your health needs change as you grow. Some effects from cancer treatment can show up years later. You need to know what to watch for and how to get help. Here’s a quick look at common long-term health outcomes:
Health Outcome | Description |
|---|---|
Physical Issues | Surgery can affect muscle and bone growth, especially in younger children. |
Mental Health | Survivors may experience anxiety, depression, and fear of recurrence. |
Cognitive Effects | Treatments can lead to memory and learning difficulties. |
Hearing/Vision Problems | Certain treatments can cause hearing loss and vision issues. |
Cardiotoxicity | Some treatments can lead to heart problems later in life. |
Lung Issues | Certain therapies can harm lung tissue, causing breathing problems. |
Secondary Cancers | Increased risk of developing new cancers due to previous treatments. |
You may feel anxious about follow-up appointments or worry about cancer coming back. Some survivors have trouble with memory or learning new things. These challenges make it important to stay connected with doctors who understand your history.
Building Independence
The Transition to Adult Care for Childhood Cancer Survivors helps you become more independent. You start making choices about your health. Many survivors feel nervous about taking charge, but you can do it. Parents often want to help, but they also need to let you try things on your own. You build confidence by talking with your care team and asking questions. Over time, you learn to manage appointments, medicines, and health records. This step-by-step process makes you ready for adult life.
You may feel unprepared at first.
Parents support you but also give you space.
Good communication helps you feel confident.
Preventing Gaps in Care
You want to avoid missing important checkups or treatments. Gaps in care can happen when you switch from pediatric to adult doctors. Sometimes, survivors stay with their childhood care team. Others move to a new doctor or clinic. Barriers like not knowing about late effects or not wanting to leave your old team can make things harder. Take a look at this chart to see how survivors move through the system and what challenges they face:
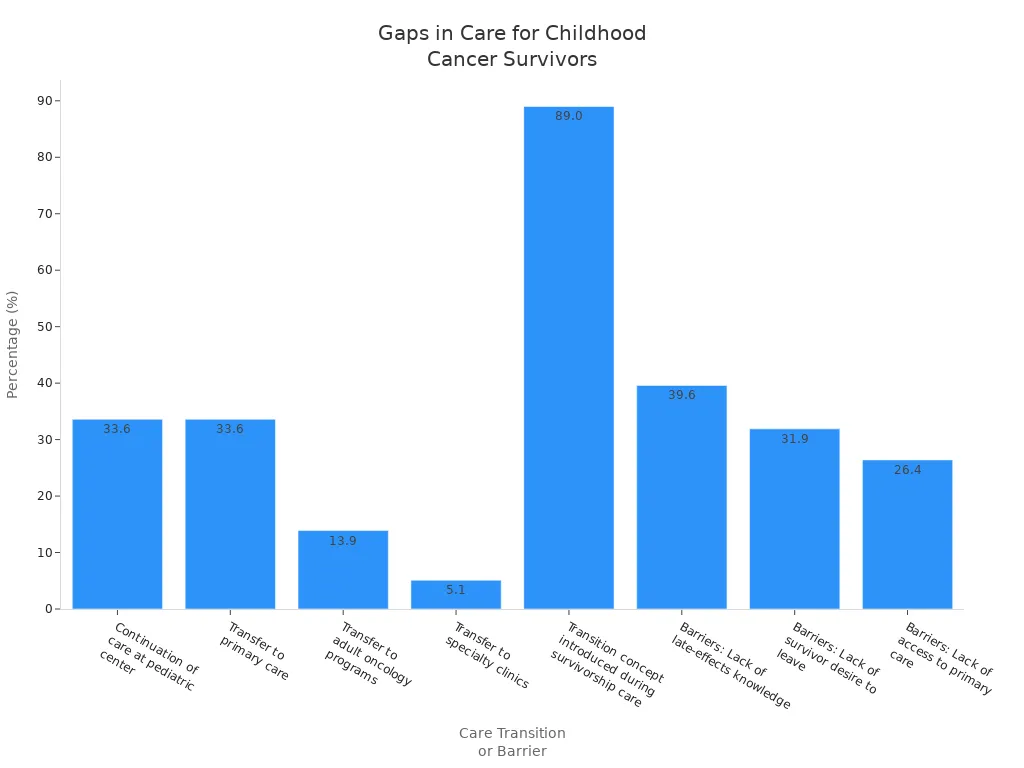
You can lower your risk of missing care by learning about your health and planning ahead. The Transition to Adult Care for Childhood Cancer Survivors gives you the tools to stay healthy and strong.
Transition Steps for Childhood Cancer Survivors

Start Early with Planning
You might think you have plenty of time before you need to switch to adult care, but starting early makes everything easier. Most experts recommend beginning to learn self-advocacy skills around age 12. This gives you time to get comfortable talking about your health and asking questions. Early planning helps you and your family feel ready for the changes ahead.
Here’s a simple list of steps to help you get started:
Develop a survivorship care plan that matches your cancer type and treatment.
Schedule regular checkups and tests to watch for late effects or cancer coming back.
Get support for any long-term side effects you might have.
Find counseling or psychosocial support if you need it.
Ask for help with legal or financial questions.
Work with different specialists to cover all your health needs.
Make healthy choices, like eating well and staying active.
Involve your family in your care and learn together.
Tip: The earlier you start planning, the more confident you’ll feel when it’s time to move to adult care.
Create a Transition Plan
A good transition plan acts like a roadmap for your health journey. It helps you keep track of your medical history and what you need to do next. Your plan should include a few key parts:
Component | Description |
|---|---|
A record of your treatment history and your personal health needs. | |
Follow-Up Plan | A written plan that lists your cancer type, treatments, possible long-term effects, and tips for staying healthy. |
Psychosocial Support | Information about support for your emotions, growth, and relationships. |
You can use this plan to share important details with your new adult care team. It also helps you remember what to watch for as you get older.
Develop Self-Advocacy Skills
Learning to speak up for yourself is a big part of The Transition to Adult Care for Childhood Cancer Survivors. You need to know how to ask questions, share your concerns, and make decisions about your health. Start practicing these skills early so you feel ready when you meet new doctors.
Here are some important self-advocacy skills:
Strategy | Description |
|---|---|
Communication | Practice telling your doctors and nurses what you need and how you feel. |
Information-Seeking | Look for answers about your health and treatments. |
Problem-Solving | Figure out what to do when you face a challenge or a new health problem. |
Negotiation | Work with your care team and family to make choices that fit your needs. |
Note: Knowing your own needs and values helps you stand up for yourself and get the care you deserve.
Select Adult Care Providers
Choosing the right adult care provider is a big step. You want someone who understands your history and listens to your concerns. Your pediatric oncologist can help you find a good match. Look for a provider who works well with both primary care doctors and cancer specialists. This teamwork makes sure you get the best care possible.
Criteria for Selecting Adult Care Providers | Description |
|---|---|
Doctors work together to cover all your health needs. | |
Provider Experience | Choose someone who has cared for other cancer survivors. |
Communication and Coordination | Good communication between your old and new doctors is key. |
Survivor Characteristics | Your age, gender, and background can help you find the right provider. |
Provider Comfort | Pick a doctor who feels confident treating childhood cancer survivors. |
Quality of Life and Satisfaction | Your happiness and health matter most when picking a provider. |
Tip: Ask your pediatric team for recommendations and meet with new providers before you make a decision.
Maintain Continuity of Care
You want your care to feel smooth and connected, not broken up or confusing. The Transition to Adult Care for Childhood Cancer Survivors works best when everyone stays in touch and shares information. Your pediatric oncologist plays a big role in preparing you for this change. They can help you understand your medical history and what to expect from adult care.
Here are some ways to keep your care on track:
Start learning about aftercare while you’re still with your pediatric team.
Visit your new adult care provider before you leave pediatric care.
Make sure your doctors talk to each other and share your records.
Ask for help if you feel lost or confused about the new system.
Keep a list of your medicines, allergies, and important health facts.
Remember: Regular check-ins and open communication between your old and new care teams help you stay healthy and confident.
The Transition to Adult Care for Childhood Cancer Survivors can feel like a big step, but with early planning, a strong transition plan, and the right support, you can move forward with confidence.
Overcoming Transition Challenges
Insurance and Coverage Issues
You might notice that insurance changes can make things tricky during your move to adult care. Sometimes, your coverage changes right when you need it most. If you did not have insurance when you were first diagnosed, you may get coverage later but still face problems getting care. Some survivors face extra barriers because of their race, ethnicity, or family income. These challenges can make it harder to get the follow-up visits you need.
Issue | What It Means |
|---|---|
Insurance Coverage Change | Your insurance might change, which can affect your doctor visits. |
Uninsurance Impact | Getting insurance later helps, but you may still have trouble getting care. |
Disparities in Care | Some groups have a harder time getting the care they need. |
Tip: Ask your care team or social worker for help understanding your insurance options.
Communication Barriers
You may feel confused when your doctors do not talk to each other. Sometimes, your pediatric and adult doctors do not share information well. This can make you feel lost or worried. You might also notice that your parents, doctors, and you do not always agree or understand each other. These relationship issues can make the transition harder.
Doctors may not share your medical history.
You, your parents, and your doctors may not always communicate well.
General doctors and cancer specialists sometimes do not work together.
If you feel unsure, ask questions and speak up about your needs.
Emotional and Psychological Support
You might feel a mix of emotions during The Transition to Adult Care for Childhood Cancer Survivors. You could feel happy that treatment is over, but also scared or sad. Some survivors worry about cancer coming back. Others feel stress at checkups or sadness about missing out on parts of childhood. You might even feel guilty for surviving when others did not.
You can get support in many ways:
Emotional support from friends, family, or support groups
Academic help if school feels hard
Psychotherapy or counseling
Psychiatric services for bigger emotional needs
Remember, it is okay to ask for help. You are not alone.
Managing Complex Medical Histories
Your medical history might feel long and complicated. You may need to learn new ways to manage your health. Some survivors do not know enough about their past treatments or the health problems they might face later. You could have ongoing issues like tiredness or trouble thinking clearly. These problems can last a long time and need regular care.
Challenge | What You Can Do |
|---|---|
Self-management | Learn how to keep track of your health and speak up for yourself. |
Knowledge of late effects | Ask your doctors to explain your medical history and risks. |
Chronic late effects | Get help for ongoing problems like fatigue or memory issues. |
Keep a notebook or use an app to track your health and questions for your doctors.
Support and Resources for Survivors
Tools for Transition
You have access to some great tools that make moving to adult care easier. These tools help you keep track of your health and remind you about important appointments. You can share your medical history with new doctors and stay organized. Here’s a quick look at some helpful options:
Tool Name | Description |
|---|---|
Passport for Care | Creates a personalized Survivorship Care Plan based on your treatment. You can store it safely and share it with your family. |
SurvivorLink™ | Lets you upload and organize health documents in a secure online record. You can share these with your healthcare providers. |
Electronic reminders | Sends you reminders about upcoming care. These help you remember follow-up visits and keep your health on track. |
Tip: Try using these tools early. You’ll feel more confident and prepared for each step.
Organizations and Networks
You don’t have to go through The Transition to Adult Care for Childhood Cancer Survivors alone. Many organizations and networks offer support, resources, and guidance. You can reach out to these groups for help, advice, or just someone to talk to.
Organization | Description | Population Served | Contact Information |
|---|---|---|---|
Survivorship Program Resource Center — Children's Cancer Cause | Childhood cancer survivors | ||
ACTS Program at Rady Children’s Health | Gives care and education about long-term effects. | Survivors two years off therapy, up to age 26 | Lilibeth Torno, MD ltorno@choc.org |
Dana-Farber/Boston Children’s Center | Improves care through specialized clinics. | Survivors diagnosed before age 40 | Rusha Bhandari, MD, MS rbhandari@coh.org |
Aflac Survivor Program at CHOA | Supports long-term follow-up and transition. | Survivors under 21, or older if treated at CHOA | Karen Effinger, MD, MS Karen.effinger@emory.edu |
Penn State Health Survivorship Program | Offers transition programs and telemedicine. | Survivors two years off therapy, up to age 30 | Smita Dandekar, MD sdandekar@pennstatehealth.psu.edu |
You can ask your care team to help you connect with these organizations.
Educational Materials
You need the right information to feel ready for your next steps. Educational materials help you understand your health and what to expect. Here are some things you should keep in mind:
Keep a copy of your treatment summary and survivorship care plan.
Continue lifelong follow-up care to watch for late effects.
Ask your care team, family, or friends for recommendations for adult care providers.
Be honest with your new healthcare provider about any symptoms or changes.
Use support from family, friends, and support groups.
Remember to set up a survivorship care plan with your cancer care team. Include checks for late effects, referrals to specialists, and tips for healthy living.
You can use these resources to make your transition smoother and stay healthy as you grow.
Improving the Transition Model
Current Gaps in Care
You might notice that the transition process does not look the same everywhere. Many families feel unsure about what comes next. Some hospitals do not have a clear plan for moving you from pediatric to adult care. You may find that doctors do not always talk to each other. Sometimes, you do not get enough information about your treatment or future checkups. You may also miss out on support services that help you feel confident.
Here is a table showing some common gaps in care:
Gap in Care | Description |
|---|---|
Lack of Awareness | Families often do not know about psychosocial services. |
Access Barriers | Distance and busy schedules make it hard to get resources. |
Need for Tailored Support | Survivors and families want support that fits their needs. |
You may want more details about your health, like a summary of your treatments or a schedule for follow-up visits. Sometimes, you wish for more help from providers who understand your history. You might also see that some survivors get better support than others, depending on where they live.
There is no universal model for transition.
You may not get enough guidance or support.
Doctors sometimes lack experience with survivor care.
Communication between teams can be weak.
Future Directions
You can expect changes in the way care teams help you move forward. Researchers are working to improve the transition process. They focus on teaching you about your health and building your skills for managing care. You may see new programs that offer emotional support and help you learn how to coordinate your own care.
Here is a table showing what experts are studying:
Description | |
|---|---|
Knowledge Delivery | Helps you learn about your health and care needs. |
Skill Development | Teaches you how to manage appointments and records. |
Psychosocial Needs | Supports your feelings and social life during transition. |
Need for High-Quality Studies | Calls for better research to guide future programs. |
You will benefit from stronger teamwork between pediatric and adult care providers. When doctors share your medical history and talk to each other, you get better care. You may also see more training for providers who work with survivors. Some countries, like Canada, help survivors build self-management skills early. Others, like Switzerland, encourage parents to stay involved. These differences show that each system can learn from others.
Early preparation helps you feel ready.
Self-management training gives you confidence.
Collaboration between care teams keeps your care connected.
New models will focus on your needs and make transitions smoother.
The Transition to Adult Care for Childhood Cancer Survivors will keep improving as more people share ideas and research. You can look forward to a future where your care feels safe, connected, and easy to manage.
You can make The Transition to Adult Care for Childhood Cancer Survivors smoother by planning early and working with your care team. Take a look at the benefits you get from proactive planning:
Benefit Description | How It Helps You |
|---|---|
Connects you with experts for long-term follow-up | |
Support for AYA survivors | Gives you help with school and healthcare systems |
Uninterrupted care | Improves your quality of life |
Working together with your family and doctors makes your care stronger. Teams that talk and share information help you feel safe and supported.
Ask for better training for providers.
Support national standards for transitions.
Help others by sharing your experience.
FAQ
What age should you start planning for the transition to adult care?
You should start learning about your health and planning for adult care around age 12. Early planning gives you time to build confidence and learn new skills.
How do you find the right adult care provider?
Ask your pediatric team for recommendations. Meet with new doctors before you switch. Look for someone who listens and understands your history.
What if you feel nervous about leaving your pediatric team?
It’s normal to feel nervous. Talk to your family and care team about your worries. They can help you feel more comfortable and answer your questions.
Do you need to keep your survivorship care plan after switching doctors?
Yes! Keep your survivorship care plan. It helps your new doctors understand your history and gives you a record of your treatments and follow-up needs.
#BanishCancer
See Also
Simplifying The Basics Of B-Cell Prolymphocytic Leukemia
Exploring The Nature Of Chronic Lymphocytic Leukemia
Decoding Large Cell Lung Carcinoma With Rhabdoid Features
Treatment Approaches For Acute Myeloid Dendritic Cell Leukemia

