Top Breakthroughs in Cancer Prevention and Treatment Research
Recent breakthroughs in cancer research have revolutionized how you prevent, detect, and treat the disease. Early detection tools now save lives by identifying cancer in its earliest stages. For example, advanced algorithms have improved diagnostic accuracy by nearly 10%, ensuring faster and more reliable results. Secondary prevention efforts have cut cancer-related mortality by up to 20%, showing the power of proactive measures. Additionally, studies reveal that early detection of colorectal and lung cancers saves billions in healthcare costs, proving its economic and medical value. These trends in cancer prevention research: what’s new, continue to transform outcomes and offer hope to millions.
Key Takeaways
New tests, like liquid biopsies, help find cancer early. This improves survival and lowers medical costs.
Studying genes, like polygenic risk scores, shows who might get cancer. This helps stop cancer before it starts.
Living healthy can stop up to half of cancers. Easy habits, like exercising and eating well, really help.
Special cancer vaccines and immunotherapy treat tumors by boosting the immune system and targeting bad cells.
New tools, like carbon ion therapy, treat tough cancers better and more accurately.
Trends in Cancer Prevention Research: What’s New
Advances in Genetic Research for Cancer Risk Assessment
Genetic research has transformed how you assess cancer risk. Scientists now use advanced tools like polygenic risk scores (PRS) and DNA methylation markers to identify individuals at higher risk. For example, PRS studies have shown that men in the top quintile of risk scores are over twice as likely to develop prostate cancer compared to those with average scores. Similarly, DNA methylation markers improve early detection of lung cancer by up to 8% when combined with traditional models. These breakthroughs allow you to take proactive steps, such as enhanced screening or lifestyle changes, to reduce your risk.
Researchers are also exploring multi-omics integration, which combines genetic variations and methylation changes. This approach improves prediction models for high-risk populations, especially for diseases like lung cancer. By understanding your genetic predisposition, you can make informed decisions about prevention and early intervention.
Early Detection Technologies Revolutionizing Screening
Early detection remains one of the most effective ways to combat cancer. New technologies like liquid biopsies and multi-cancer early detection (MCED) tests are changing the game. For instance, the CancerSEEK test detected early-stage cancers in 65% of cases during a study involving over 10,000 women. Another test, Cancerguard, demonstrated a specificity of 98.5%, ensuring fewer false positives. These advancements mean you can detect cancer earlier, increasing the chances of successful treatment.
Emerging trends in cancer prevention research also focus on improving accessibility. Researchers are working on non-invasive methods that require minimal effort from patients, such as blood-based tests. These innovations aim to make screening more convenient and widely available, ensuring that more people benefit from early detection.
Lifestyle Interventions Backed by Research
Your lifestyle choices play a significant role in cancer prevention. Studies show that up to 50% of cancers are preventable through healthy habits. For example, adhering to a Mediterranean diet can lower your cancer risk by 7% for every increase in adherence score. Regular physical activity reduces cancer mortality by 13%, while higher-intensity exercises cut breast cancer risk by 27%. Even small changes, like using aspirin regularly, can reduce colorectal cancer risk by 20-40%.
A healthy lifestyle doesn’t just lower your risk; it also improves overall well-being. Avoiding tobacco, maintaining a balanced diet, and staying active are simple yet powerful strategies. By making these changes, you can significantly reduce your chances of developing cancer and improve your quality of life.
Tip: Start small. Incorporate one healthy habit at a time, like adding more fruits and vegetables to your meals or taking a daily walk. Over time, these small steps can lead to big health benefits.
Innovations in Cancer Treatment

Personalized Cancer Vaccines and Precision Oncology
Personalized cancer vaccines represent a groundbreaking approach to treatment. These vaccines target unique mutations, known as neoantigens, in your tumor cells. By stimulating your immune system to recognize and attack these mutations, they aim to prevent recurrence and improve survival rates. For example, the PGV001 vaccine demonstrated strong immune responses in a phase I trial involving 13 patients across multiple cancer types. At a five-year follow-up, six patients were alive, and three remained tumor-free.
Clinical trials have shown promising results across various cancer types:
Cancer Type | Trial Phase | Key Findings |
|---|---|---|
Non-small cell lung cancer (NSCLC) | Phase I | 60% of participants could receive the vaccine; 83% showed systemic T cell responses. |
Follicular lymphoma | N/A | Synthetic long peptide vaccines successfully treated all enrolled patients. |
Metastatic melanoma | Phase Ib | Strong immunogenic responses and robust safety profile with NOUS-PEV vaccine and pembrolizumab. |
Triple-negative breast cancer | Phase I | 87.5% recurrence-free survival at 36 months; 78% developed specific immune responses. |
Metastatic soft tissue sarcoma | Pilot study | Stable disease up to 208 days; 50% showed de novo T-cell responses against neoantigens. |
These vaccines are part of precision oncology, which tailors treatments to your genetic profile. This approach ensures therapies are more effective and less toxic, improving your quality of life during treatment.
Note: Personalized cancer vaccines are still in early stages of development, but their potential to transform cancer care is immense.
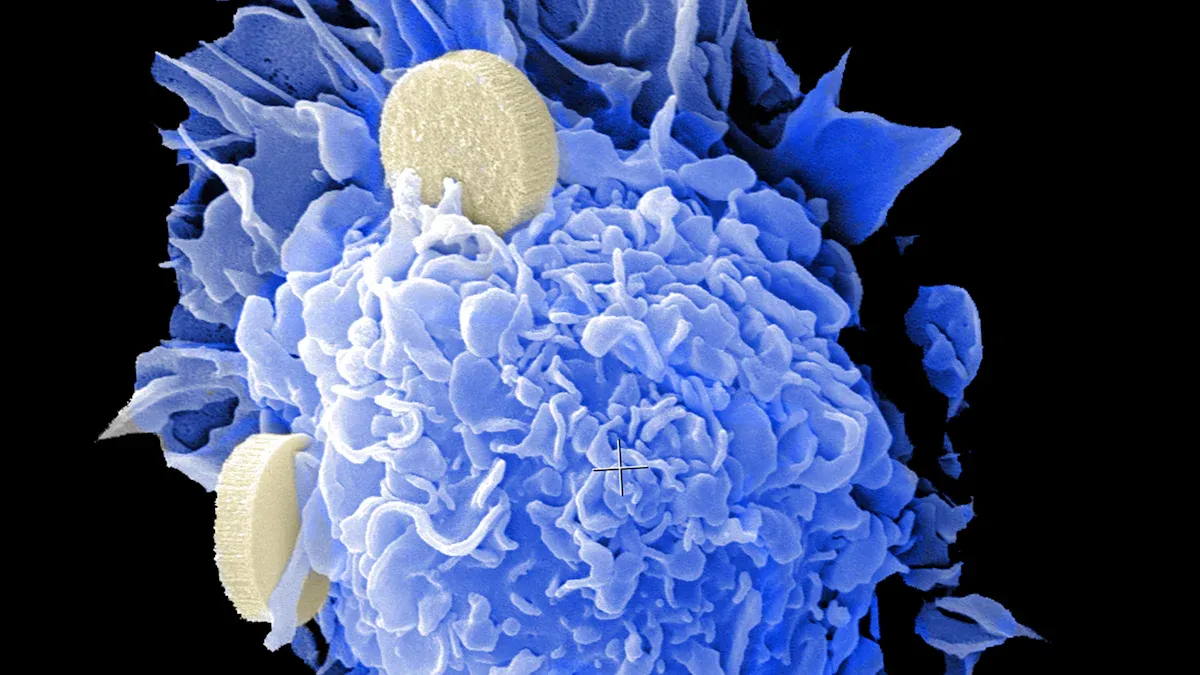
Immunotherapy: Harnessing the Immune System
Immunotherapy has revolutionized cancer treatment by leveraging your immune system to fight the disease. Treatments like checkpoint inhibitors and CAR-T cell therapy have shown remarkable success in improving survival rates. For instance, the phase III KEYNOTE-204 trial revealed that pembrolizumab achieved a median progression-free survival (PFS) of 13.2 months compared to 8.3 months for brentuximab vedotin in relapsed Hodgkin lymphoma patients.
Here’s how different immunotherapy protocols compare:
Treatment Group | Objective Response Rate (ORR) | Progression-Free Survival (PFS) | Overall Survival (OS) |
|---|---|---|---|
IO + IO | 42.18% vs. 27.8% | 7.80 months vs. 5.70 months | 30.2 months vs. 16.8 months |
Anti-PD-(L)1 Monotherapy | 21.5% vs. 17.4% | 3.12 months vs. 4.24 months | 12.3 months vs. 9.6 months |
Anti-PD-(L)1 + Chemotherapy | 48.2% vs. 32.4% | N/A | 17.9 months vs. 12.6 months |
Anti-PD-(L)1 + CTLA-4 | 50.0% vs. 23.0% | 11.5 months vs. 5.65 months | 72.1 months vs. 22.9 months |
Anti-PD-(L)1 + TKI | 53.1% vs. 30.8% | 15.93 months vs. 9.40 months | N/A |
Cumulative | 42.5% vs. 26.1% | 8.55 months vs. 5.53 months | 26.8 months vs. 17.2 months |
Immunotherapy doesn’t just improve survival rates; it also enhances your quality of life by reducing the need for invasive procedures. With advancements in this field, you can expect more effective and personalized treatments in the future.
Seven-Minute Cancer Treatment Jab: A Game-Changer
Imagine receiving your cancer treatment in just seven minutes. This is now possible thanks to a revolutionary injection developed for immunotherapy. Administered subcutaneously, this jab delivers the same medication as traditional intravenous infusions but in a fraction of the time.
The seven-minute jab is particularly beneficial for patients undergoing immunotherapy with atezolizumab, a checkpoint inhibitor used to treat various cancers, including lung and bladder cancer. By reducing treatment time, this innovation minimizes your discomfort and frees up valuable resources in healthcare settings.
Tip: If you’re considering immunotherapy, ask your healthcare provider about this new option. It could make your treatment experience more convenient and less stressful.
This breakthrough highlights the ongoing efforts to improve cancer care, making treatments faster, more accessible, and patient-friendly.
Carbon Ion Radiotherapy: Enhancing Treatment Efficacy
Carbon ion radiotherapy (CIRT) is emerging as one of the most advanced forms of cancer treatment. Unlike traditional photon-based radiation, carbon ions deliver higher precision and greater biological effectiveness. This means you can target tumors more accurately while minimizing damage to surrounding healthy tissues. For patients with hard-to-treat cancers, such as those resistant to conventional therapies, CIRT offers a promising alternative.
One of the key advantages of carbon ion therapy lies in its ability to cause complex DNA damage in cancer cells. Studies show that carbon ions produce more DNA double-strand breaks compared to photons. These breaks are harder for cancer cells to repair, leading to higher rates of cell death. Additionally, carbon ion therapy triggers a stronger immune response by activating the cGAS-STING pathway. This pathway detects damaged DNA in the cytoplasm and signals your immune system to attack the cancer. As a result, you benefit from both direct tumor destruction and enhanced immune activity.
Here’s how carbon ions compare to other radiation types:
Property | Carbon Ions | Protons | Photons |
|---|---|---|---|
1.2 - 3.5 | 1.1 | N/A | |
Oxygen Enhancement Ratio | Low (more effective in hypoxic conditions) | N/A | N/A |
Immune Response | More robust | N/A | N/A |
Lateral Scattering | Reduced | N/A | N/A |
Bragg Peak-to-Entrance Dose Ratio | Higher | N/A | N/A |
The table highlights why carbon ions stand out. Their higher RBE means they are more effective at killing cancer cells, even in low-oxygen environments where other treatments often fail. Reduced lateral scattering ensures that the radiation stays focused on the tumor, sparing nearby healthy tissues. This precision makes CIRT particularly effective for cancers located near critical organs, such as the brain or spinal cord.
Another benefit of carbon ion therapy is its ability to treat radioresistant tumors. These are cancers that don’t respond well to traditional radiation. With carbon ions, you can overcome this resistance, giving you a better chance at successful treatment. For example, patients with sarcomas or pancreatic cancer have shown improved outcomes with CIRT compared to conventional methods.
Note: Carbon ion radiotherapy is currently available in select treatment centers worldwide. If you’re exploring advanced options, consult with your healthcare provider to see if this therapy is right for you.
As research continues, the potential of carbon ion therapy grows. Its ability to combine precision targeting with immune activation could redefine how you approach cancer treatment. For patients seeking cutting-edge solutions, CIRT offers hope and a path forward.
The Role of Artificial Intelligence
AI in Early Detection and Diagnosis
Artificial intelligence (AI) has transformed how you detect and diagnose cancer. AI-based tools analyze medical data to identify abnormalities earlier and more accurately than traditional methods. For example:
AI improves adenoma detection rates during colonoscopy by 30–50%.
Adenoma detection rates with AI reach 29.6%, compared to 19.3% without AI.
Polyp detection rates increase to 45.4% with AI versus 30.6% without AI.
These advancements mean you can benefit from earlier interventions, which improve treatment outcomes. AI also serves as a second opinion for radiologists, reducing false positives and enhancing diagnostic accuracy. It even detects precancerous polyps with over 90% accuracy, outperforming conventional methods.
AI doesn’t just stop at detection. It analyzes tumor progression and treatment responses, helping doctors make better decisions. With AI, you gain access to tools that enhance precision and reliability in cancer diagnosis.
AI for Treatment Optimization and Predictive Analytics
AI plays a critical role in optimizing cancer treatment plans. By analyzing patient data, genetic information, and treatment responses, AI enables personalized care. This reduces trial-and-error approaches and boosts clinical confidence.
Studies highlight AI’s impact:
Study | Findings |
|---|---|
Del Giorgio Solfa et al. | AI improves diagnostic accuracy and treatment planning for better outcomes. |
Wolinetz and Tabak | Machine-learning models enhance early predictions for cancer treatment. |
Schroeder and Lodemann | AI predicts outcomes like acute kidney injury, enabling timely interventions. |
AI frameworks also predict responses to immunotherapy with accuracy rates of 70–90%. These predictive analytics improve healthcare outcomes by up to 35%, ensuring you receive tailored treatments that work best for you.
Machine Learning Tools for Long-Term Outcome Prediction
Machine learning (ML) tools help predict long-term outcomes in cancer care. These models use data-driven approaches to classify diseases and forecast recovery. For example:
SAFIRE and SAHIT models predict functional recovery in patients with aneurysmatic subarachnoid hemorrhage.
ML algorithms like Extreme Gradient Boosting and Random Forest predict severe outcomes in COVID-19 patients with diabetic ketoacidosis.
Wearable devices and personalized care systems also use ML to monitor your health and coordinate treatments. These tools provide insights into recovery timelines and help doctors plan interventions. By leveraging ML, you gain access to smarter healthcare solutions that focus on your long-term well-being.
Future Directions in Cancer Research
Emerging Trends in Cancer Prevention and Screening
Cancer prevention and screening are evolving rapidly, driven by new technologies and research. Molecular technologies, such as advanced 'omics' approaches, now allow scientists to create detailed molecular profiles of cancer. These profiles help identify potential therapeutic targets, giving you access to more precise prevention strategies. Precision medicine is also gaining momentum. By using predictive biomarkers, doctors can tailor screening and prevention plans to your unique genetic makeup, reducing unnecessary procedures.
Artificial intelligence (AI) is another game-changer. AI tools analyze large datasets to improve early detection and screening accuracy. For example, AI can identify abnormalities in imaging scans that might go unnoticed by the human eye. However, challenges remain. A recent study comparing screening guidelines from top cancer centers and the USPSTF revealed inconsistencies, particularly for breast, prostate, and cervical cancers. This highlights the need for uniform policies to balance the benefits of early detection with the risks of overdiagnosis.
Challenges in Advancing Cancer Treatment
Cancer treatment faces significant hurdles. Tumor heterogeneity, or the variation within tumors, complicates treatment because different parts of a tumor may respond differently to the same therapy. Tumor evolution adds another layer of complexity. As cancer cells mutate, they often develop resistance to drugs, making it harder to maintain effective treatment. Additionally, limited research on residual disease—cancer cells that remain after treatment—hinders progress in precision medicine.
These challenges underscore the importance of ongoing research. Scientists are exploring ways to overcome drug resistance and improve treatment for hard-to-treat cancers. By addressing these issues, you can expect more effective therapies in the future.
Promising Areas for Future Exploration
The future of cancer research holds immense promise. Scientists are focusing on innovative therapies like CAR-T cell therapy, which has shown success in treating blood cancers such as leukemia and lymphoma. Antibody-drug conjugates (ADCs) are another exciting development. These therapies deliver toxic drugs directly to tumor cells, minimizing harm to healthy tissues.
Other promising areas include cancer vaccines, which aim to prevent and treat cancer, and CRISPR technology, which allows precise gene editing to correct mutations. Oncolytic virus therapy is also gaining attention. This approach uses viruses to selectively infect and destroy cancer cells while boosting your immune system.
Advancements in radiation therapy, such as proton and heavy ion therapy, offer more precise targeting of tumors, reducing damage to surrounding tissues. By combining these cutting-edge treatments with AI-driven diagnostics, you can look forward to a future where cancer care is more personalized and effective.
The breakthroughs in cancer prevention and treatment have reshaped how you approach this disease. From early detection tests identifying 95% of pancreatic cancers to CAR-T-cell therapy achieving remission for over a decade, these advancements offer hope.
Breakthrough | Evidence |
|---|---|
CAR-T-cell therapy | 12 years remission for two patients; 19 years remission for a patient treated at age four |
Early pancreatic cancer detection test | Identifies 95% of early pancreatic cancers |
Breast cancer risk drug | Could halve the chance of developing breast cancer for 300,000 women |
These innovations have also transformed survival rates. For example, targeted therapies like imatinib have extended life expectancy for chronic myeloid leukemia (CML) patients from 2.5 years to decades.
Time Period | Average Survival (CML) | Treatment Type |
|---|---|---|
25 years ago | 2.5 - 3 years | Traditional therapies |
Present | Decades | Targeted therapies (e.g., imatinib) |
Recent years | Improved outcomes | Immunotherapies (e.g., pembrolizumab) |
These advancements not only improve survival but also enhance your quality of life. As research progresses, you can look forward to more personalized, effective, and accessible cancer care. The future of cancer research holds immense promise, offering hope to millions worldwide.
FAQ
What is the most promising breakthrough in cancer treatment today?
Personalized cancer vaccines stand out as a major breakthrough. These vaccines target specific mutations in your tumor cells, boosting your immune system to fight cancer effectively. Clinical trials show promising results, especially for hard-to-treat cancers.
How does AI improve cancer detection?
AI analyzes medical data to identify cancer earlier and more accurately. For example, AI tools improve polyp detection rates during colonoscopies by up to 50%. This ensures you benefit from earlier interventions, which significantly improve treatment outcomes.
Are lifestyle changes enough to prevent cancer?
Lifestyle changes can reduce your cancer risk by up to 50%. Eating a balanced diet, staying active, and avoiding tobacco are key. Research shows that even small changes, like regular exercise, can lower breast cancer risk by 27%.
What makes carbon ion radiotherapy unique?
Carbon ion radiotherapy delivers precise, high-energy radiation that targets tumors while sparing healthy tissues. It’s especially effective for cancers resistant to traditional treatments. This therapy also triggers a stronger immune response, enhancing its effectiveness.
Can cancer be cured completely?
Some cancers, like certain leukemias, can achieve long-term remission with treatments like CAR-T cell therapy. However, many cancers remain chronic conditions. Ongoing research aims to develop more effective therapies, offering hope for better outcomes.
See Also
Recognizing Symptoms And Treatment Options For Duodenal Cancer
An In-Depth Overview Of Various Types Of Cancer
Exploring Cancer Types Associated With AIDS Infection

