Understanding B-cell prolymphocytic leukemia made simple
B-cell prolymphocytic leukemia is a rare form of leukemia that progresses aggressively. It accounts for fewer than 1% of all leukemia cases involving lymphocytes. This disease disrupts the production of healthy blood cells by causing an overproduction of abnormal B-cells. Without timely treatment, it can lead to life-threatening complications. Most cases occur in individuals aged 65 to 69, with a median survival of 30 to 50 months. Its rapid progression makes early detection and prompt medical care essential for improving outcomes.
Key Takeaways
B-cell prolymphocytic leukemia (B-PLL) is a rare blood cancer. It mostly affects older adults between 65 and 69 years old.
Finding it early is very important. Symptoms include feeling very tired, getting sick often, and swollen lymph nodes. Early treatment helps.
Treatments include chemotherapy, immunotherapy, and stem cell transplants. These can help people feel better and live longer.
Changes in certain genes, like MYC and TP53, affect how the disease grows. These changes also guide doctors in choosing treatments.
Talking to doctors and using helpful resources can support patients and families in handling B-PLL well.
What is B-cell prolymphocytic leukemia?
Definition and classification
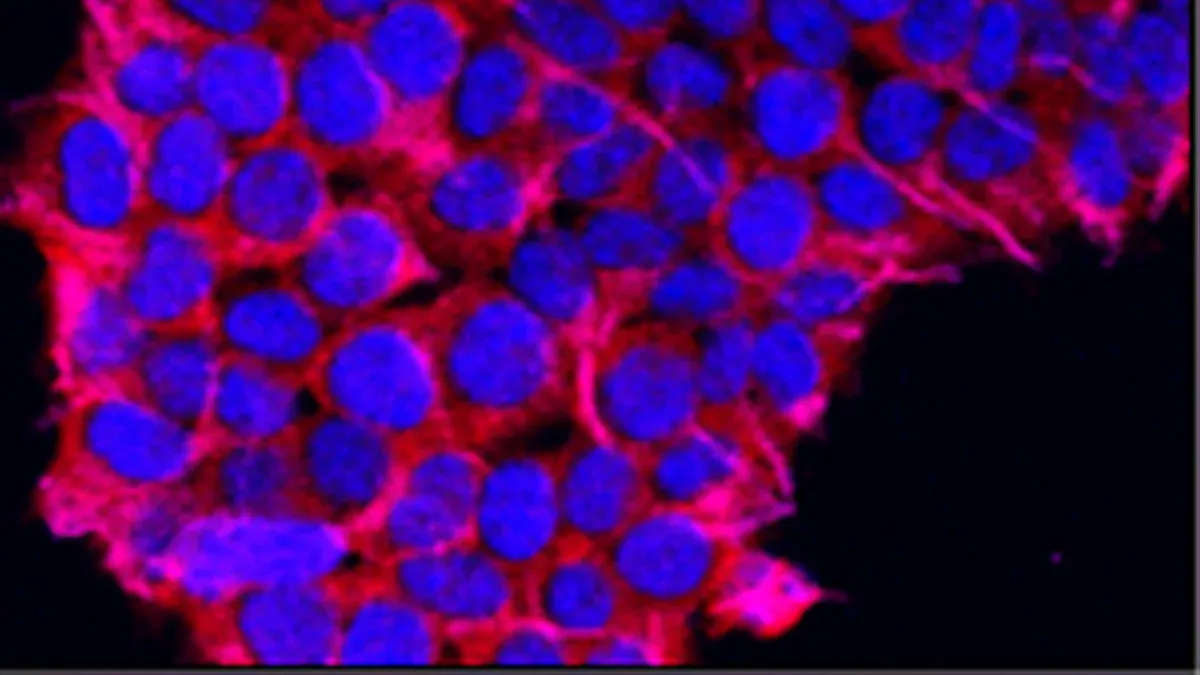
B-cell prolymphocytic leukemia is a rare and aggressive type of leukemia that develops from B lymphocytes, a type of white blood cell responsible for producing antibodies. It accounts for less than 1% of all B-cell leukemias. Unlike chronic lymphocytic leukemia (CLL), which progresses slowly, this disease advances rapidly and requires immediate medical attention.
Previously, B-cell prolymphocytic leukemia was considered a subtype of CLL. However, it is now classified as a distinct condition due to its unique features. For example, it typically presents with more than 55% prolymphocytes (immature B cells) in the blood, a characteristic that sets it apart from CLL. In some cases, B-PLL may develop as a progression of CLL, while in others, it appears as a new (de novo) disease.
Key characteristics of B-PLL
B-cell prolymphocytic leukemia stands out due to its aggressive nature and rapid progression. Here are some defining features:
It primarily affects mature B cells, causing them to divide uncontrollably.
The excessive growth of these abnormal cells crowds out healthy blood cells, leading to symptoms like fatigue, infections, and easy bruising.
B-PLL has a high recurrence rate and generally poorer outcomes compared to other types of leukemia.
It shares some genetic similarities with mantle cell lymphoma (MCL), another type of B-cell cancer.
You may wonder how B-PLL differs from other leukemias. While it affects B cells, T-cell prolymphocytic leukemia (T-PLL) targets T cells. B-PLL is also more common than T-PLL, though both are rare. Compared to CLL, B-PLL progresses faster and has a less favorable prognosis.
Understanding these characteristics can help you recognize the seriousness of this condition and the importance of early diagnosis.
Symptoms of B-cell prolymphocytic leukemia
Common symptoms
When you have B-cell prolymphocytic leukemia, you may notice a range of symptoms that affect your daily life. These symptoms often result from the overproduction of abnormal B-cells, which disrupt the normal functioning of your blood and immune system. Here are some of the most common symptoms:
Fatigue, which affects 70–80% of patients, often due to anemia.
Fever or night sweats, experienced by 20–30% of individuals.
Unintentional weight loss, reported by 30–40% of patients.
Enlarged lymph nodes, also known as lymphadenopathy, seen in 50–60% of cases.
An enlarged spleen (splenomegaly), which occurs in 80–90% of patients and may cause abdominal discomfort.
An enlarged liver (hepatomegaly), affecting 30–40% of individuals.
Frequent infections due to a weakened immune system.
Easy bruising or bleeding, caused by low platelet counts.
These symptoms can vary in severity, but they often worsen as the disease progresses. If you experience any of these signs, it’s important to consult a healthcare professional promptly.
How symptoms progress
The symptoms of B-cell prolymphocytic leukemia tend to worsen over time as the disease advances. Early on, you might feel fatigued or notice swollen lymph nodes. As the abnormal B-cells multiply, they crowd out healthy blood cells, leading to more severe issues.
Symptom | Prevalence (%) | Description |
|---|---|---|
Fatigue | 70–80 | Caused by anemia, leading to persistent exhaustion. |
Splenomegaly | 80–90 | Enlarged spleen causing abdominal discomfort and early satiety. |
Recurrent infections | 50–60 | Weakened immune system increasing susceptibility to infections. |
Easy bruising | 40–50 | Low platelet count affecting blood clotting, resulting in bruising or bleeding. |
Fever | 20–25 | Reaction to leukemia cells or infections, signaling disease progression. |
As the disease progresses, you may experience more frequent infections, severe fatigue, and significant weight loss. Enlarged organs like the spleen or liver can cause discomfort or pain. These changes highlight the importance of early detection and treatment to manage symptoms effectively.
Causes and risk factors of B-cell prolymphocytic leukemia
Genetic mutations and other causes
B-cell prolymphocytic leukemia often develops due to specific genetic mutations. These mutations disrupt the normal functioning of B-cells, leading to their uncontrolled growth. Research shows that mutations in the MYC and TP53 genes are particularly common in this disease. In fact, about 76% of patients with B-PLL exhibit abnormalities in the MYC gene. Other frequently affected genes include MYD88, BCOR, and several others. These genetic changes play a critical role in the disease's progression and may influence treatment options.
Environmental factors can also contribute to the development of leukemia, including B-PLL. Prolonged exposure to chemicals like benzene or ionizing radiation increases your risk. Lifestyle choices, such as smoking, may further elevate this risk. However, having these risk factors does not guarantee that you will develop the disease. Most individuals with these exposures never experience leukemia.
Note: Understanding the genetic and environmental causes of B-PLL can help you and your healthcare provider explore targeted treatment options.
Risk factors like age and gender
Certain risk factors make you more likely to develop B-cell prolymphocytic leukemia. These include:
Being male.
Being older, as the median age of diagnosis is 69 years.
Having a family history of leukemia or other blood cancers.
B-PLL is most commonly diagnosed in individuals over the age of 60, with the average age at presentation between 65 and 70 years. Men are more frequently affected than women. While these factors increase your risk, they do not guarantee that you will develop the disease.
By understanding these risk factors, you can stay informed and seek medical advice if you notice any concerning symptoms. Early detection remains key to managing B-PLL effectively.
Diagnosing B-cell prolymphocytic leukemia
Diagnostic tests
Diagnosing B-cell prolymphocytic leukemia involves several specialized tests. These tests help identify abnormal B-cells and confirm their characteristics. Your doctor may recommend the following diagnostic procedures:
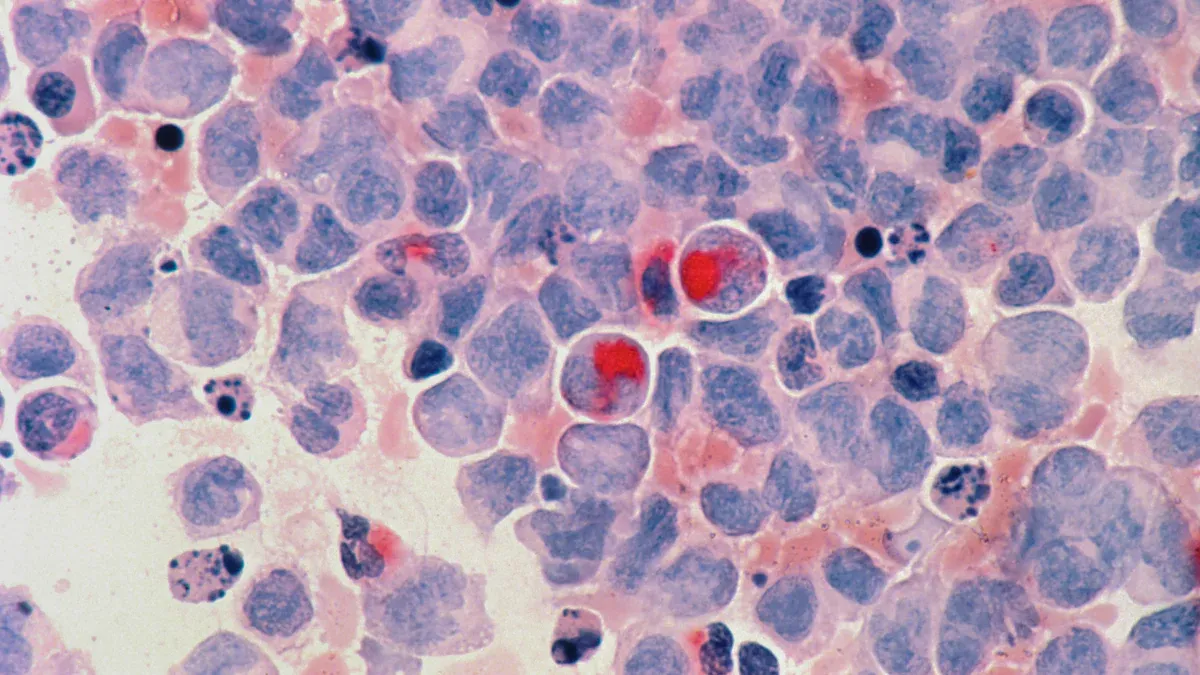
Peripheral blood smear: This test examines your blood under a microscope to detect abnormal prolymphocytes.
Bone marrow biopsy: A small sample of your bone marrow is taken to assess the presence of leukemia cells.
Immunophenotyping: This test identifies specific markers on the surface of B-cells, helping to distinguish B-PLL from other blood cancers.
Genetic testing: This detects mutations in genes like MYC or TP53, which are often linked to B-PLL.
Cytogenetic tests: These analyze chromosomal abnormalities that may contribute to the disease.
Doctors also measure your absolute B lymphocyte count. A count of 5000 or more per microliter of blood, combined with specific B-cell markers, strongly suggests B-PLL.
Note: No single test can confirm B-PLL. Specialists often use a combination of these methods to make an accurate diagnosis.
Confirming a B-PLL diagnosis
To confirm B-cell prolymphocytic leukemia, doctors rely on specific criteria. These include the percentage of prolymphocytes in your blood and the results of advanced lab tests.
Criteria | Description |
|---|---|
Prolymphocyte Percentage | Prolymphocytes must make up more than 55% of lymphoid cells in your blood. |
Histology | Positive histology findings, with or without genetic and immunophenotyping. |
Immunophenotyping | Identifies unique markers on B-cells to confirm the diagnosis. |
Absolute B Lymphocyte Count | A count of 5000 or more per microliter, with mostly mature-appearing lymphocytes. |
Clonality | Demonstration of clonality in B-cells is required. |
Diagnosing B-PLL can be challenging because it shares features with other blood cancers like chronic lymphocytic leukemia and mantle cell lymphoma. Specialists use multiple tests to differentiate between these conditions. This thorough approach ensures you receive the most accurate diagnosis and appropriate treatment.
Treatment options for B-cell prolymphocytic leukemia

Standard treatments
Treating B-cell prolymphocytic leukemia often involves a combination of therapies tailored to your specific condition. Here are the most common options:
Chemotherapy: Doctors frequently use drugs like fludarabine, cyclophosphamide, and rituximab to kill cancer cells.
Immunotherapy: Monoclonal antibodies, such as rituximab and alemtuzumab, help your immune system target and destroy abnormal B-cells.
Targeted Therapy: Medications like ibrutinib and venetoclax focus on specific proteins that cancer cells need to grow and survive.
Stem Cell Transplantation: This procedure replaces diseased bone marrow with healthy stem cells, offering a potential cure for some patients.
Clinical Trials: These provide access to experimental treatments that may improve outcomes.
Each treatment has unique benefits and risks. For example, chemotherapy can cause side effects like fatigue and nausea, while stem cell transplants are complex and require careful consideration.
Emerging therapies
New therapies are showing promise in treating B-cell prolymphocytic leukemia. Drugs like ibrutinib and venetoclax target proteins essential for cancer cell survival. Ibrutinib blocks a protein that helps B-PLL cells grow and divide, while venetoclax disrupts a protein that allows these cells to survive.
Other emerging options include:
Idelalisib (Zydelig): A drug that inhibits pathways critical for cancer cell growth.
CAR-T Cell Therapy: A cutting-edge approach where your T-cells are modified to attack cancer cells.
These therapies are still under investigation but have already demonstrated encouraging results in clinical trials.
Managing symptoms and supportive care
Managing symptoms is crucial for improving your quality of life during treatment. You can take several steps to support your overall well-being:
Maintain a nutritious diet: Focus on fruits, vegetables, whole grains, and lean proteins to keep your body strong.
Engage in light physical activity: Activities like walking or yoga can reduce fatigue and improve circulation.
Manage stress effectively: Techniques like meditation or deep breathing can enhance mental health.
Prioritize quality sleep: Rest allows your body to recover and maintain energy levels.
Prevent infections: Practice good hygiene and stay up to date on vaccinations to reduce risks.
Tip: Always consult your healthcare provider before making lifestyle changes to ensure they align with your treatment plan.
Prognosis and outlook for B-cell prolymphocytic leukemia
Survival rates and influencing factors
The prognosis for B-cell prolymphocytic leukemia depends on several factors, including your age, overall health, and how well you respond to treatment. On average, the median survival time is less than three years. However, some patients live longer if their disease responds well to therapy.
Here’s a breakdown of survival probabilities over time:
Time (Years) | Survival Probability |
|---|---|
3 | 63% |
5 | 56% |
10 | 35% |
Several factors can influence your prognosis:
Age: Older individuals may face a poorer outlook compared to younger patients.
Overall health: Pre-existing conditions can make treatment more challenging.
Response to treatment: A strong response to therapy often leads to better outcomes.
Disease progression: Rapidly advancing disease typically results in a shorter survival time.
Genetic mutations: Abnormalities in genes like MYC and TP53 can negatively impact prognosis.
Your doctor may use genetic testing to identify these mutations and tailor your treatment plan accordingly.
Importance of early detection
Early detection plays a critical role in managing B-cell prolymphocytic leukemia. Identifying the disease in its initial stages allows your healthcare team to start treatment before symptoms worsen. This can improve your quality of life and potentially extend survival.
You should monitor for symptoms like fatigue, frequent infections, or an enlarged spleen. If you notice these signs, consult a healthcare professional promptly. Early diagnosis often involves blood tests, bone marrow biopsies, and genetic testing. These tools help confirm the disease and guide treatment decisions.
By staying vigilant and seeking medical advice early, you can take proactive steps to manage this aggressive condition effectively.
B-cell prolymphocytic leukemia is a rare but aggressive disease that demands early detection and swift treatment. Understanding its symptoms, causes, and treatment options empowers you and your family to make informed decisions. Key takeaways include its rarity, primarily affecting older adults, and its rapid progression, which often leads to a challenging prognosis.
Tip: Consulting healthcare professionals ensures you receive personalized care. Treatments like chemotherapy, targeted therapies, and stem cell transplants can improve your quality of life and outcomes.
To stay informed, explore resources like expert webinars, podcasts, and educational materials. These tools can deepen your understanding and help you navigate this complex condition effectively.
FAQ
What makes B-cell prolymphocytic leukemia different from other leukemias?
B-PLL progresses faster than most leukemias, including chronic lymphocytic leukemia (CLL). It also involves a higher percentage of prolymphocytes in the blood. These differences make it more aggressive and challenging to treat.
Can B-cell prolymphocytic leukemia be cured?
Currently, there is no guaranteed cure for B-PLL. However, treatments like chemotherapy, targeted therapies, and stem cell transplants can help manage the disease and improve your quality of life.
How is B-PLL diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic testing to diagnose B-PLL. They look for specific markers, such as a high percentage of prolymphocytes and genetic mutations like MYC or TP53.
Is B-PLL hereditary?
B-PLL is not typically hereditary. However, a family history of leukemia or other blood cancers may increase your risk. Genetic mutations linked to B-PLL usually occur spontaneously rather than being inherited.
What should you do if you suspect B-PLL?
If you notice symptoms like fatigue, frequent infections, or an enlarged spleen, consult a doctor immediately. Early diagnosis and treatment can improve your prognosis and help manage symptoms effectively.
Tip: Keep track of your symptoms and share them with your healthcare provider for a more accurate diagnosis.
See Also
A Simple Guide to Understanding Acute Biphenotypic Leukemia
An Easy Explanation of Acute Myeloid Leukemia
A Clear Overview of AIDS Related Lymphoma
Anaplastic Large Cell Lymphoma: Definition and Treatment Options
Treatment Approaches for Acute Myeloid Dendritic Cell Leukemia

