Understanding Diffuse Large B-Cell Lymphoma
Diffuse large B-cell lymphoma is an aggressive form of non-Hodgkin lymphoma. It accounts for about 22% of newly diagnosed B-cell non-Hodgkin lymphoma cases in the U.S. and represents roughly one-third of all lymphomas. Despite its aggressive nature, this condition is treatable, especially when diagnosed early. Early treatment significantly improves survival rates. For instance, patients diagnosed at stage 1 have a survival rate of 79.2%. Recognizing symptoms and seeking timely medical care can make a critical difference in outcomes.
Key Takeaways
Diffuse large B-cell lymphoma (DLBCL) is a fast-growing cancer. It can be treated well, especially if found early. Early care can greatly improve chances of survival.
Look for symptoms like swollen lymph nodes, night sweats, or weight loss. See a doctor quickly if you notice these signs.
Knowing the types of DLBCL, like Germinal Center B-Cell and Activated B-Cell, helps in talking about treatments with your doctor.
New treatments, like CAR T-cell therapy and targeted drugs, bring hope. Ask your doctor about these options if cancer comes back.
Regular check-ups are important after treatment to stay healthy. Learning more and staying active in your care can help you feel better.
What is Diffuse Large B-Cell Lymphoma?
Overview of DLBCL
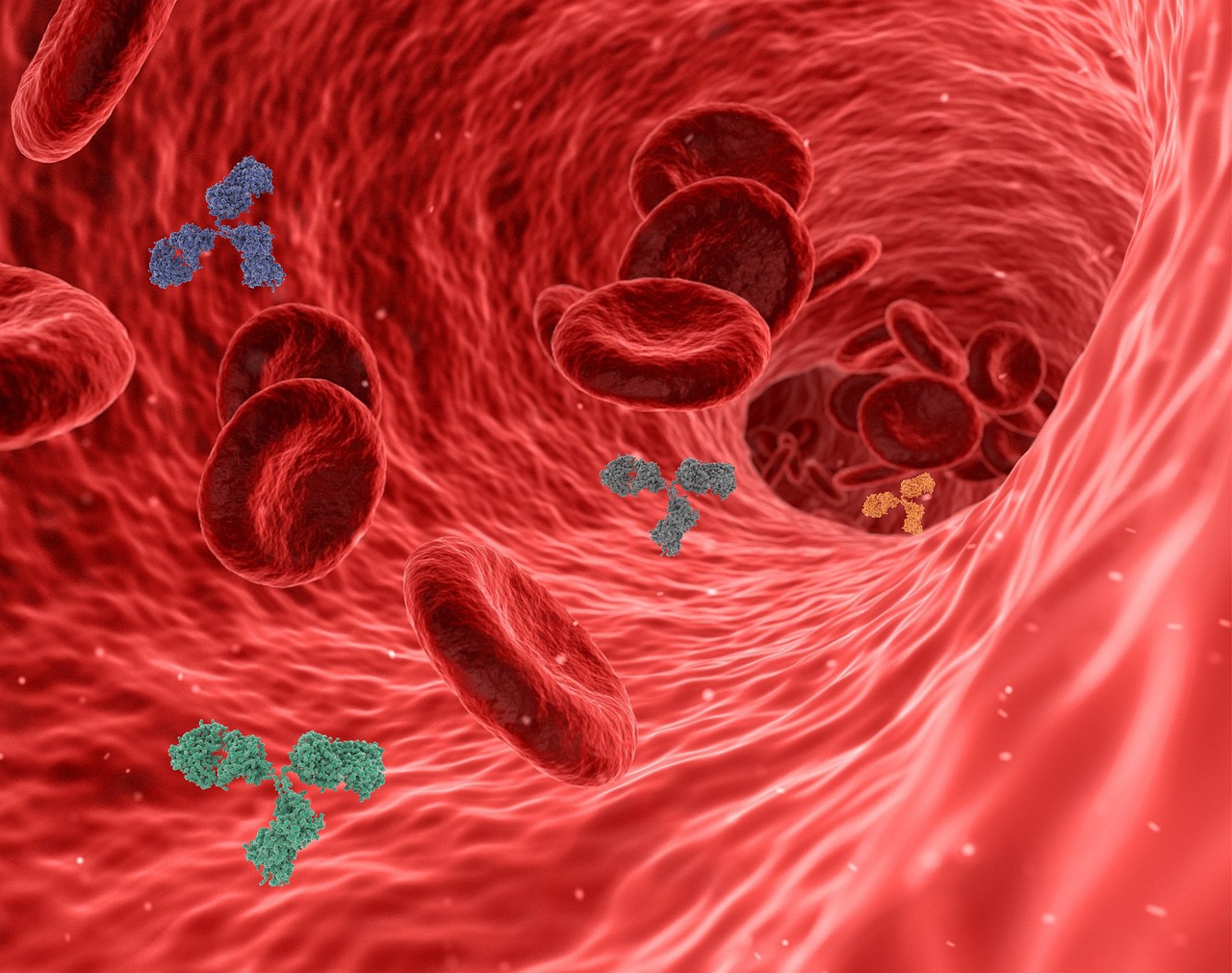
Diffuse large B-cell lymphoma is the most common type of non-Hodgkin lymphoma, making up about 22% of newly diagnosed cases in the United States. This aggressive cancer affects B-lymphocytes, which are essential for your immune system to fight infections. Unlike other lymphomas, it can develop in lymph nodes or extranodal sites, such as the stomach, skin, or brain. Under a microscope, the malignant B cells appear larger than normal ones and do not clump together. This unique characteristic reflects the disease's aggressive nature. Despite its rapid growth, it often responds well to treatment, with many patients achieving remission after therapy.
How DLBCL Develops
Diffuse large B-cell lymphoma develops when genetic mutations transform normal B cells into cancerous ones. These mutations disrupt the processes that regulate cell growth and survival. For example, B-cell receptor signaling and the activation of NF-kappaB play key roles in promoting the survival and proliferation of these malignant cells. Chronic infections, such as those caused by Epstein-Barr virus (EBV) or Helicobacter pylori, can also increase the risk of developing this lymphoma. These infections stimulate your immune system, leading to increased lymphocyte production and a higher chance of genetic errors.
Subtypes of DLBCL
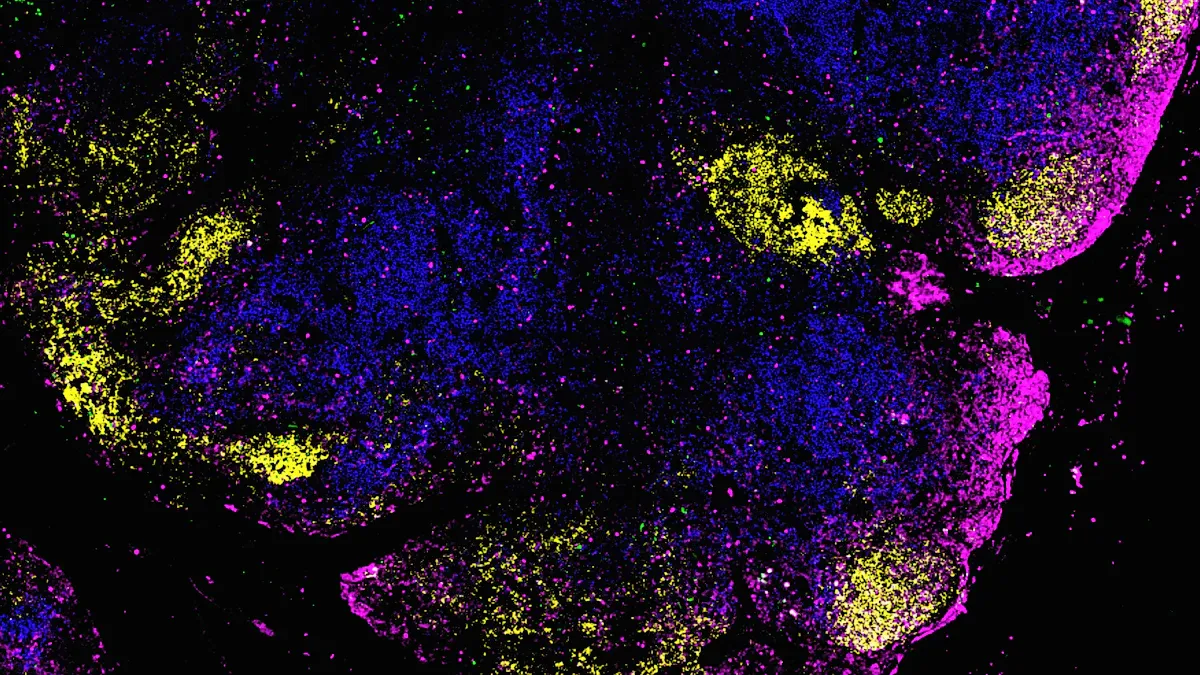
Germinal Center B-Cell (GCB) Subtype
The GCB subtype originates from B cells in the germinal center of lymph nodes. It is the most common subtype and is associated with better treatment outcomes. This subtype often responds well to rituximab-based therapies due to the deregulation of the Bcl-6 gene. Patients with GCB-DLBCL generally have a higher overall survival rate compared to other subtypes.
Activated B-Cell (ABC) Subtype
The ABC subtype is less common but more challenging to treat. It is characterized by high NF-kappaB activity, which makes the cancer cells more resistant to standard therapies. This subtype also shows overexpression of specific genes linked to poor clinical outcomes. Patients with ABC-DLBCL often require advanced treatment strategies to improve their prognosis.
Symptoms of Diffuse Large B-Cell Lymphoma
Recognizing the symptoms of Diffuse Large B-Cell Lymphoma early can help you seek timely medical care. Symptoms may vary depending on the stage of the disease and the organs affected.
Common Symptoms
You might notice several general symptoms that are common in many cases of Diffuse Large B-Cell Lymphoma. These include:
Swollen lymph nodes, often painless and located in the neck, armpits, or groin.
Drenching night sweats that disrupt your sleep.
Fevers that come and go without an obvious cause.
Unexplained weight loss, even when your diet hasn’t changed.
Persistent itching that doesn’t seem to have a clear source.
These symptoms, often referred to as "B symptoms," can signal the aggressive nature of the disease. If you experience any of these, it’s important to consult a healthcare provider promptly.
Symptoms Based on Organ Involvement
When Diffuse Large B-Cell Lymphoma spreads to specific organs, the symptoms can vary. Here’s a breakdown of how symptoms differ based on the affected area:
Organ Affected | Symptoms |
|---|---|
Abdominal lymphoma | Stomach pain, diarrhea, bleeding |
Chest lymphoma | Shortness of breath, pain, cough, headaches |
For example, if the lymphoma develops in your abdomen, you might feel persistent stomach pain or notice changes in your bowel habits, such as diarrhea. Bleeding in the digestive tract can also occur. On the other hand, lymphoma in the chest can lead to breathing difficulties, chest pain, or a persistent cough. In some cases, headaches may also develop due to pressure in the chest area.
By understanding these symptoms, you can better monitor your health and seek medical advice if needed. Early detection plays a crucial role in improving outcomes for Diffuse Large B-Cell Lymphoma.
Causes and Risk Factors of Diffuse Large B-Cell Lymphoma
Causes of DLBCL
Diffuse large B-cell lymphoma develops due to a combination of genetic and environmental factors. Genetic mutations in B cells disrupt their normal growth and survival, leading to uncontrolled cell division. These mutations often affect pathways like NF-κB, which plays a key role in cell proliferation. Chronic infections, such as Epstein-Barr virus (EBV), can also contribute. EBV activates oncogenic pathways through proteins like latent membrane protein 1 (LMP-1), which mimics signals that promote cell survival. This virus can immortalize B cells, increasing the likelihood of lymphoma development.
Environmental factors also play a role. Exposure to chemicals, such as pesticides or industrial solvents, has been linked to higher risks. Smoking and obesity are additional contributors. A personal history of cancer or organ transplantation further increases susceptibility, as these conditions weaken the immune system.
Risk Factors
Age and Gender
Your risk of developing this lymphoma increases with age. It is most common in individuals over 60. Men are more likely to develop the disease than women and often experience worse outcomes.
Family History of Lymphoma
Having a first-degree relative with lymphoma slightly raises your risk. About 9% of patients with this condition report a family history of non-Hodgkin lymphoma.
Immune System Disorders
Autoimmune diseases, such as rheumatoid arthritis or lupus, weaken your immune system. This makes you more vulnerable to developing lymphoma. Organ transplant recipients, who take immunosuppressive drugs, also face a significantly higher risk.
Infections like Epstein-Barr Virus (EBV)
Certain infections, including EBV, can transform normal lymphocytes into cancerous cells. EBV-positive lymphomas often show specific genetic changes that promote cancer growth. Other infections, such as HIV or hepatitis viruses, also increase your risk.
Risk Factor | Description |
|---|---|
Environmental Exposures | Chemicals and radiation exposure raise the risk of lymphoma. |
Body Weight | Obesity is linked to a higher likelihood of developing this disease. |
Cigarette Smoking | Long-term smoking contributes to the risk of lymphoma. |
Understanding these causes and risk factors can help you take steps to monitor your health and reduce potential risks.
Diagnosis of Diffuse Large B-Cell Lymphoma
Medical History and Physical Exam
Diagnosing diffuse large B-cell lymphoma begins with your doctor reviewing your medical history and performing a physical exam. They will ask about symptoms like swollen lymph nodes, fever, or weight loss. During the exam, they will check for enlarged lymph nodes in areas such as your neck, armpits, or groin. They may also examine your abdomen and chest for signs of organ involvement. This initial step helps guide further diagnostic testing.
Diagnostic Tools
Biopsy of Lymph Nodes or Affected Tissue
A biopsy is the most reliable way to confirm a diagnosis. Your doctor may recommend an excisional biopsy, where the entire lymph node is removed for analysis. If this is not possible, multiple core biopsies can provide enough tissue for evaluation. Pathologists examine the sample under a microscope to identify cancerous cells. Flow cytometry and cytogenetic studies may also be used to determine the lymphoma's subtype and genetic characteristics.
Diagnostic Tool | Description |
|---|---|
Lymph Node Biopsy | Primary method for diagnosis, confirmed by pathology findings. |
Excisional Biopsy | Preferred procedure unless contraindicated; core biopsies are acceptable. |
Flow Cytometry | Identifies immunophenotypes to differentiate between B- and T-cell origins. |
Cytogenetic/FISH Studies | Reveals chromosomal translocations characteristic of DLBCL. |
Imaging Tests (CT, PET Scans)
Imaging tests play a crucial role in staging and evaluating the extent of the disease. A CT scan identifies enlarged lymph nodes and extranodal involvement. PET scans detect areas of high metabolic activity, which often indicate cancer. These scans help your doctor determine the stage of the lymphoma and plan treatment.
Imaging Test | Role in DLBCL Diagnosis |
|---|---|
CT Scans | Identify lymphadenopathy and extranodal disease; part of complete staging workup. |
PET Scans | Indicate metabolic activity associated with lymphoma; used for staging through FDG uptake. |
Blood Tests and Bone Marrow Biopsy
Blood tests provide additional information about your overall health. They measure levels of red and white blood cells, platelets, and lactate dehydrogenase (LDH), which can indicate disease activity. A bone marrow biopsy may be necessary to check if the lymphoma has spread to your bone marrow. This involves extracting a small sample of bone marrow tissue for examination.
Early and accurate diagnosis is essential for effective treatment. If you notice symptoms, consult your doctor promptly.
Treatment Options for Diffuse Large B-Cell Lymphoma
Standard Treatments
Chemotherapy (e.g., R-CHOP regimen)
Chemotherapy remains the cornerstone of treatment for Diffuse Large B-Cell Lymphoma. The most common protocol is the R-CHOP regimen, which combines four chemotherapy drugs with a monoclonal antibody. This regimen includes:
Cyclophosphamide
Doxorubicin
Vincristine
Prednisone
Rituximab (Rituxan)
Doctors typically administer R-CHOP in cycles every three weeks. For early-stage cases, you may receive 3 to 6 cycles, sometimes followed by radiation therapy. For advanced stages, R-CHOP continues to be the first-line treatment, offering significant remission rates.
Radiation Therapy
Radiation therapy targets specific areas where lymphoma is localized. It is often used after chemotherapy for early-stage disease or to manage symptoms in advanced cases. This approach helps reduce tumor size and alleviate discomfort caused by swollen lymph nodes or organ involvement.
Advanced Treatments
Targeted Therapies (e.g., Monoclonal Antibodies)
Targeted therapies focus on specific molecules involved in cancer growth. Recent advancements include:
Advancement | Description |
|---|---|
Replaces vincristine in R-CHOP, approved for intermediate- to high-risk patients. | |
CAR T-cell therapy | Uses genetically modified T cells to attack lymphoma, approved as second-line therapy. |
Bispecific antibodies | Drugs like epcoritamab and glofitamab show high response rates in relapsed cases. |
These therapies offer hope for patients with relapsed or refractory Diffuse Large B-Cell Lymphoma, especially when standard treatments are less effective.
Stem Cell Transplantation
Stem cell transplantation provides another option for patients with relapsed or high-risk disease. This procedure involves replacing damaged bone marrow with healthy stem cells. Autologous transplants, which use your own cells, are the most common type. This approach can help restore normal blood cell production after intensive chemotherapy.
Clinical Trials and Emerging Therapies
Clinical trials explore new treatments and combinations to improve outcomes. Current studies include:
Trial Name | Description |
|---|---|
Compares this drug with standard immunochemotherapy. | |
CAR T-cell Therapy Trials | Assess the efficacy of CAR T-cell therapy in relapsed/refractory cases. |
Glofitamab Study | Evaluates glofitamab combined with chemotherapy. |
Selinexor Combination Study | Tests selinexor with other drugs for relapsed/refractory lymphoma. |
Participating in a clinical trial gives you access to cutting-edge therapies that may not yet be widely available. Discuss these options with your doctor to determine if a trial is right for you.
Advances in treatment have significantly improved outcomes for Diffuse Large B-Cell Lymphoma. Whether you pursue standard therapies or explore emerging options, early and personalized care remains essential.
Prognosis and Living with Diffuse Large B-Cell Lymphoma
Prognosis Factors
International Prognostic Index (IPI) score
The International Prognostic Index (IPI) score helps doctors predict outcomes for patients with Diffuse large B-cell lymphoma. This tool categorizes you into one of four risk groups based on factors like age, disease stage, performance status, LDH levels, and the number of extranodal sites involved. Patients in the low-risk group have a 5-year survival rate of 73%, while those in the high-risk group have a survival rate of 26%. Understanding your IPI score can guide treatment decisions and set realistic expectations for recovery.
Response to Treatment
Your response to treatment significantly impacts your prognosis. Achieving complete remission after initial therapy improves long-term survival rates. Patients who respond well to first-line treatments like the R-CHOP regimen often have better outcomes. However, if the disease relapses, advanced therapies such as CAR T-cell therapy or stem cell transplantation can offer hope for remission.
Coping with DLBCL
Managing Side Effects
Treatment for Diffuse large B-cell lymphoma can cause side effects like fatigue, nausea, and hair loss. To manage these, you can:
Stay hydrated and eat nutrient-rich foods to maintain energy levels.
Use prescribed medications to control nausea and other symptoms.
Rest when needed but stay active to improve overall well-being.
Discuss any side effects with your doctor to adjust your treatment plan if necessary.
Emotional and Psychological Support
Living with lymphoma can be emotionally challenging. You may feel fear, sadness, or anxiety. To cope, consider these strategies:
Spend time outdoors to reduce stress and improve your mood.
Practice yoga or meditation to enhance emotional resilience.
Lean on friends and family for support.
Listen to music to relax and uplift your spirits.
Acknowledging your emotions and seeking help when needed can make a big difference in your mental health.
Long-Term Outlook
The long-term outlook for patients in remission is promising. Studies show that 80.7% of patients remain in remission two years after treatment, while 13.2% experience a relapse. Regular follow-ups with your doctor are essential to monitor your health and address any concerns promptly. Advances in treatment continue to improve survival rates, offering hope for a brighter future.
Diffuse large B-cell lymphoma is a treatable condition, especially when diagnosed early. Acting quickly can significantly improve survival rates. For example, patients who begin treatment within 22 days of diagnosis have better outcomes, with a progression-free survival rate of 75.9%. Recent advancements, such as CAR T-cell therapy, offer hope for patients with relapsed disease, achieving potential cure rates of 30-40%. Innovations like the POLARIX trial have also improved progression-free survival by refining chemotherapy regimens. These breakthroughs highlight the importance of seeking timely medical care and exploring advanced treatment options. Always consult your doctor for personalized guidance.
Diagnosis-to-Treatment Interval (DTI) | Overall Survival (OS) | Progression-Free Survival (PFS) |
|---|---|---|
Short DTI (0–22 days) | 62.7% | 55.1% |
Long DTI (over 22 days) | 86.4% | 75.9% |
Early diagnosis and modern therapies have transformed the outlook for this aggressive lymphoma. By staying informed and proactive, you can take control of your health journey.
FAQ
What is the survival rate for Diffuse Large B-Cell Lymphoma?
The survival rate depends on factors like stage and treatment. Early-stage patients have a 5-year survival rate of about 73%. Advanced treatments, such as CAR T-cell therapy, improve outcomes for relapsed cases. Always consult your doctor for personalized information.
Can Diffuse Large B-Cell Lymphoma spread to other organs?
Yes, it can spread to organs like the liver, lungs, or brain. This is called extranodal involvement. Symptoms vary based on the affected organ. For example, abdominal involvement may cause pain, while chest involvement can lead to breathing difficulties.
Are there any lifestyle changes that can help during treatment?
Yes, maintaining a healthy diet, staying hydrated, and engaging in light physical activity can help. These steps improve energy levels and overall well-being. Discuss any lifestyle changes with your doctor to ensure they align with your treatment plan.
Is Diffuse Large B-Cell Lymphoma hereditary?
A family history of lymphoma slightly increases your risk, but most cases are not hereditary. Genetic mutations and environmental factors play a larger role in its development. If you have concerns, consider genetic counseling for more insights.
What should you do if treatment side effects become severe?
Inform your doctor immediately if side effects worsen. They can adjust your treatment or prescribe medications to manage symptoms like nausea or fatigue. Never ignore severe side effects, as timely intervention ensures better comfort and recovery.
Tip: Keep a journal of your symptoms and side effects to share with your healthcare team during appointments.
See Also
A Simple Guide to B-Cell Prolymphocytic Leukemia
Key Insights Into AIDS-Related Lymphoma
Anaplastic Large Cell Lymphoma: Definition and Treatment Options

