What Drives Health Disparities in Cancer Risk

Cancer risk is not distributed equally across populations. Social, systemic, and individual factors create significant disparities, especially for marginalized communities. For example:
Black men face prostate cancer mortality rates over twice as high as White men.
Rural Appalachia sees elevated rates of colorectal, lung, and cervical cancers compared to urban areas.
Hispanic, Black, and American Indian women experience higher cervical cancer incidence, with Black women having the highest death rates.
Understanding Health Disparities and Cancer Risk requires examining these inequities and their root causes to promote health equity.
Key Takeaways
Differences in cancer risk impact underserved groups due to various causes.
Better access to check-ups and tests can lower late cancer cases.
Teaching health knowledge helps people make smart choices about care.
Fixing issues like bad air and lack of healthy food is key.
Fair healthcare rules help everyone get the care they deserve.
Understanding Health Disparities and Cancer Risk

Social Determinants of Health
Income and Socioeconomic Status
Your income and socioeconomic status play a significant role in cancer risk. Lower-income individuals often face barriers to preventive care, early detection, and treatment. Studies show that people with lower socioeconomic status experience higher rates of lung, liver, and oral cancers. Neighborhood conditions also influence health behaviors, such as access to healthy food and safe spaces for exercise, which can reduce cancer risk.
Education and Health Literacy
Education affects your ability to understand and act on health information. Limited health literacy can lead to delayed cancer screenings or mismanagement of symptoms. For example, individuals with less education may not know about cancer prevention strategies, such as quitting smoking or eating a balanced diet. Promoting health literacy can empower you to make informed decisions about your health.
Environmental and Neighborhood Factors
Where you live impacts your cancer risk. Communities with poor air and water quality expose residents to carcinogens, increasing cancer rates. Underserved neighborhoods often lack grocery stores with fresh produce, leading to unhealthy diets. Chronic stress from unsafe living conditions or social isolation further worsens health outcomes.
Systemic Barriers
Access to Healthcare
Reliable healthcare access is essential for early cancer detection. Without it, you may face late-stage diagnoses, which are harder to treat. Many underserved populations struggle to access regular screenings or affordable treatments, leading to worse outcomes.
Structural Racism and Discrimination
Institutional racism affects cancer outcomes even for those with higher incomes. Chronic stress from discrimination can weaken your immune system, making you more vulnerable to illness. Addressing these systemic issues is crucial for reducing disparities.
Medical Mistrust
Historical unethical practices in healthcare have created mistrust among marginalized groups. This mistrust can discourage you from seeking care or participating in clinical trials, limiting access to life-saving treatments.
Individual-Level Factors
Comorbidities and Preexisting Conditions
If you have chronic illnesses like diabetes or heart disease, your cancer risk may increase. These conditions can complicate treatment and recovery, making prevention even more critical.
Lifestyle and Behavioral Choices
Your daily choices, such as smoking, diet, and exercise, directly impact cancer risk. For example, smoking increases lung cancer risk, while a sedentary lifestyle contributes to obesity-related cancers. Living in areas without smoke-free policies or recreational spaces can make healthy choices harder.
Genetic and Biological Factors
Your genetic makeup also influences cancer risk. Differences in tumor biology among racial and ethnic groups can affect how cancers develop and respond to treatment. Understanding these factors can help tailor prevention and treatment strategies to your needs.
Addressing Social Determinants of Health

Reducing Socioeconomic Barriers
Expanding access to preventive care
Preventive care plays a vital role in reducing cancer risk. You can benefit from early detection and timely interventions when healthcare services are accessible. Public health data shows that targeted interventions addressing social determinants of health (SDOH) improve outcomes for underserved populations. For example, increasing access to cancer screenings, such as mammograms and colonoscopies, can significantly reduce late-stage diagnoses. Expanding community health programs and mobile clinics ensures that more people receive preventive care, especially in rural or low-income areas.
Addressing financial barriers to treatment
Financial hardship often prevents you from seeking timely cancer treatment. Low-income patients face reduced access to life-saving therapies, such as immunotherapy and surgery. A study highlights that low socioeconomic status (SES) patients are 32% less likely to undergo lung cancer surgery, the primary treatment for this disease. Addressing these disparities requires policies that reduce out-of-pocket costs and provide financial assistance programs. By removing these barriers, you can focus on recovery without the added stress of financial strain.
Evidence Type | Statistic | Description |
|---|---|---|
Cervical Cancer Screening | Adherence difference between high- and low-income countries | |
Surgery Access for Lung Cancer | OR 0.68 [0.62, 0.75] | Main treatment access disparity for low SES patients |
Improving Education and Awareness
Promoting health literacy
Health literacy empowers you to make informed decisions about your well-being. Educational programs tailored to your community can help you understand cancer risks and prevention strategies. For instance, a systematic review found that culturally tailored interventions improve HPV vaccination rates among minority groups. These programs address misconceptions and foster better communication between healthcare providers and patients. By enhancing health literacy, you can take proactive steps to reduce your cancer risk.
Increasing awareness of cancer prevention
Awareness campaigns can significantly impact your health behaviors. Initiatives like interactive cancer education tools for adolescents or obesity education curricula for Hispanic communities have shown promising results. In Appalachian Kentucky, efforts to educate middle and high school students about cancer risk factors improved their health behaviors. These examples highlight the importance of targeted education in reducing cancer disparities.
Enhancing Environmental Conditions
Reducing exposure to carcinogens
Environmental hazards, such as air pollution and radon, increase your cancer risk. In Ontario, over 90% of cancer cases linked to environmental carcinogens stem from solar UV radiation, radon, and fine particulate matter (PM2.5). Addressing these risks involves implementing policies to monitor and reduce exposure. For example, promoting radon testing in homes and regulating industrial emissions can protect you from harmful carcinogens.
Addressing food deserts and promoting nutrition
Access to nutritious food is essential for cancer prevention. Living in a food desert limits your ability to maintain a healthy diet, increasing your risk of obesity-related cancers. Community initiatives that establish farmers' markets or provide subsidies for fresh produce can improve your access to healthy options. These efforts not only reduce cancer risk but also enhance overall well-being.
Key environmental carcinogens contributing to cancer cases:
Solar UV radiation
Radon in homes
PM2.5 (fine particulate matter)
Tackling Systemic Barriers
Expanding Healthcare Access
Universal healthcare coverage
Universal healthcare coverage ensures that you can access cancer care regardless of your financial situation. When healthcare is universally available, early detection rates improve significantly. For example:
The early detection rate for all cancer types increased from 14.4% to 23.07% within five years.
Stage I cancers of the lung, thyroid, colorectum, and uterine cervix showed notable increases in detection.
Universal coverage also reduces disparities in treatment access. It allows you to receive timely care, which can prevent cancer from progressing to advanced stages. By prioritizing universal healthcare, we can save lives and reduce the burden of cancer on underserved communities.
Increasing availability of cancer screenings
Expanding cancer screening programs can help you detect cancer early, when treatment is most effective. Increased screenings could prevent thousands of deaths annually. For instance:
Cancer Type | Estimated Deaths Prevented | Additional Deaths Averted with Increased Screening |
|---|---|---|
Breast Cancer | 10,179 | 1,300 |
Cervical Cancer | 27,166 | 3,400 |
Colorectal Cancer | 74,740 | 11,000 |
By making screenings more accessible, especially in rural and low-income areas, you can benefit from early interventions that improve survival rates.
Combating Structural Racism
Training healthcare providers on cultural competence
Cultural competence training equips healthcare providers to understand and respect your unique needs. This training addresses biases and improves communication, ensuring you feel heard and valued during medical visits. Programs like the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) have shown success in reducing disparities by fostering trust and understanding between patients and providers.
Implementing anti-discrimination policies
Anti-discrimination policies in healthcare protect you from biased treatment. Studies reveal that Black and Hispanic adults often report negative experiences, such as not being believed or denied pain medication. Enforcing these policies ensures equitable care and helps eliminate barriers caused by systemic racism.
Building Trust in Healthcare
Addressing the legacy of unethical practices
Historical events, such as the Tuskegee Study and the case of Henrietta Lacks, have eroded trust in healthcare among marginalized groups. Acknowledging these injustices and implementing ethical practices can rebuild your confidence in the system. Transparent communication and community engagement are essential steps in this process.
Encouraging participation in screenings and trials
Participation in cancer screenings and clinical trials can provide you with access to advanced treatments. When healthcare providers communicate effectively and address your concerns, you are more likely to engage in these opportunities. Trust-building initiatives, such as user-friendly healthcare platforms, have proven effective in improving outcomes for at-risk populations.
By addressing systemic barriers, we can create a healthcare system that prioritizes equity and ensures better outcomes for everyone. Understanding Health Disparities and Cancer Risk requires tackling these challenges head-on to promote fairness and accessibility.
Policy and Community-Based Solutions
Promoting Diversity in Research
Increasing representation in clinical trials
Diverse representation in clinical trials ensures that treatments work effectively across all populations. When you participate in trials, researchers can better understand how different groups respond to therapies. For example, Black patients have a participation rate of 58.4%, slightly higher than White patients at 55.1%. However, many groups remain underrepresented, which limits the generalizability of findings. Increasing diversity in trials improves equity and enhances the validity of cancer research.
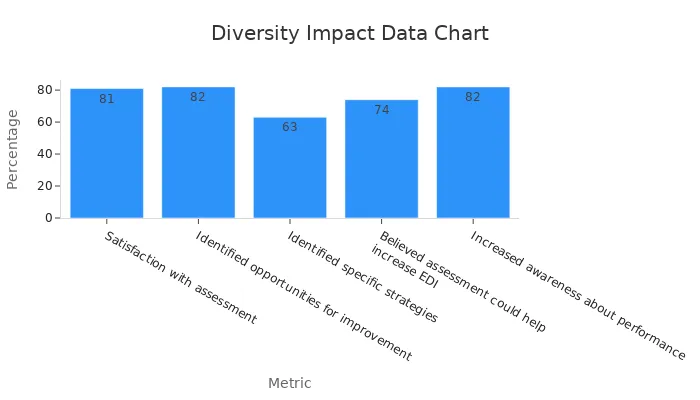
Metric | Percentage |
|---|---|
Satisfaction with assessment | 81% |
Identified opportunities for improvement | 82% |
Believed assessment could help increase EDI | 74% |
Tailoring research to population-specific risks
Cancer risks vary across populations due to genetic, environmental, and lifestyle factors. Tailored research helps address these unique risks. For instance, studies focusing on Hispanic women have identified higher cervical cancer rates, leading to targeted prevention strategies. By supporting research that considers your community's specific needs, you can benefit from more effective interventions.
Community Engagement
Partnering with local organizations
Local organizations play a critical role in addressing cancer disparities. They understand your community's unique challenges and can implement culturally tailored programs. For example, mailing fecal immunochemical test (FIT) kits with follow-up calls significantly increased screening compliance among American Indian tribes. Partnerships like these foster trust and improve access to preventive care.
Conducting education campaigns
Education campaigns raise awareness about cancer prevention and screening. Community-based education, supported by the CDC's National Comprehensive Cancer Control Program, has proven effective. Strategies like patient reminders and health worker engagement encourage you to take proactive steps. These efforts ensure you have the knowledge to make informed health decisions.
Community engagement strategies improve cancer screening rates:
Culturally tailored approaches
Mailing FIT kits with follow-ups
Patient reminders and health worker involvement
Policy Reforms
Advocating for equitable healthcare policies
Equitable healthcare policies ensure you receive the care you need, regardless of your background. Organizations like ACS CAN advocate for reducing cancer disparities by improving access to affordable healthcare. Federal funding through NIH, NCI, and CDC supports research and community programs that address structural determinants of health. These investments are vital for tackling disparities effectively.
Evidence Description | Impact on Health Disparities |
|---|---|
Federal funding through NIH, NCI, and CDC | Vital for understanding and addressing cancer disparities |
Addressing inadequate health insurance coverage | Prioritizes cancer screening for underinsured individuals |
Allocating resources to underserved areas
Policy reforms can direct resources to communities with the greatest need. Expanding Medicaid has led to earlier breast cancer detection, while community health programs have increased access to screenings and treatments. By prioritizing underserved areas, you can benefit from improved healthcare services and better outcomes.
Key policy impacts:
Earlier cancer detection through Medicaid expansion
Increased screening access via community health programs
Health disparities in cancer risk arise from a complex interplay of social, systemic, and individual factors. For example:
Black individuals face higher death rates from many cancer types compared to other groups.
People in non-metropolitan areas experience significantly higher cancer mortality than those in cities.
Education levels strongly influence cancer outcomes, with lower education linked to higher premature death rates.
Addressing these disparities requires integrated strategies. Community-based interventions, tailored communication, and collaboration across sectors can reduce risks. By prioritizing health equity and implementing global strategies like tobacco control and healthy lifestyle promotion, you can help create a future with better outcomes for all populations.
FAQ
What are health disparities in cancer risk?
Health disparities in cancer risk refer to differences in cancer rates, outcomes, and access to care among various groups. These disparities often affect marginalized communities due to factors like income, education, and systemic barriers.
How does where you live impact your cancer risk?
Your neighborhood can expose you to environmental risks like air pollution or carcinogens. Limited access to healthy food and safe spaces for exercise also increases your cancer risk. Improving these conditions can help reduce disparities.
Why is health literacy important in cancer prevention?
Health literacy helps you understand cancer risks and prevention strategies. When you know how to access screenings or adopt healthy habits, you can make informed decisions that lower your risk.
How can systemic racism affect cancer outcomes?
Systemic racism creates barriers to equitable healthcare. Discrimination and bias can lead to delayed diagnoses or inadequate treatment. Addressing these issues ensures fair access to care for everyone.
What role do lifestyle choices play in cancer risk?
Your lifestyle choices, like smoking, diet, and exercise, directly influence cancer risk. Adopting healthier habits can reduce your chances of developing cancer and improve overall well-being.
See Also
Exploring Cancer Types Associated With AIDS Infection
Understanding Lung Adenocarcinoma Causes and Associated Risks
An In-Depth Overview of Various Cancer Types

