Understanding Keratoacanthoma and Its Key Features
Keratoacanthoma is a skin tumor that grows quickly and forms a dome-shaped lesion. You may notice it resembles squamous cell carcinoma, but it is usually benign. This condition often appears on areas exposed to the sun, such as your face or hands. Interestingly, it has the potential to resolve on its own without treatment. However, early evaluation by a dermatologist is essential to confirm its nature and rule out more serious conditions.
Key Takeaways
Keratoacanthoma is a harmless skin growth that grows fast. It often looks like squamous cell carcinoma. Seeing a skin doctor early is important to know for sure.
Most keratoacanthomas show up on areas exposed to the sun, like the face and hands. Protecting your skin from sunlight can lower your chances of getting it.
Surgery is the most common way to treat keratoacanthoma. Treating it early works well and avoids problems later.
Checking your skin often and seeing a doctor for strange growths can keep your skin healthy and stop bigger problems.
Using sunscreen with SPF 30 or more and wearing sun-protective clothes are good ways to avoid keratoacanthoma and other skin issues.
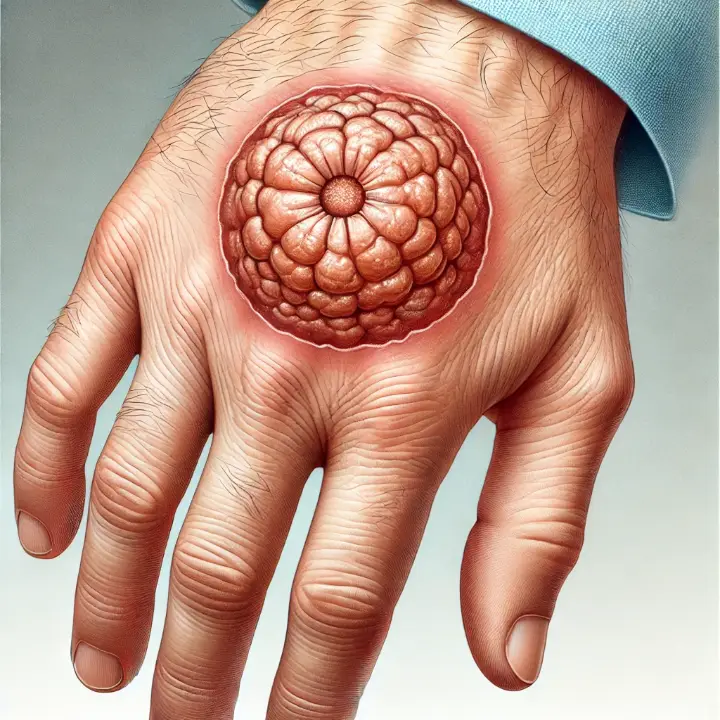
Symptoms and Characteristics of Keratoacanthoma

Key Features
Keratoacanthoma often presents as a dome-shaped lesion with a distinct central crater filled with keratin. These lesions typically grow rapidly, reaching sizes of 1-2 cm within weeks. Despite their alarming growth, they may spontaneously regress over time. Most keratoacanthomas are firm, sharply defined, and either skin-colored or erythematous. You might notice a thick crust forming over the central crater, giving it a characteristic appearance. While these lesions are usually painless, some individuals report mild itching.
Common Locations
You are more likely to find keratoacanthomas on sun-exposed areas of your body. These include the face, neck, arms, and hands. Other common sites include the ears, scalp, and lower legs. The lesions often appear on skin that has been damaged by prolonged exposure to ultraviolet (UV) rays. If you notice a rapidly growing nodule in these areas, it is essential to seek medical advice.
Differentiating Keratoacanthoma
Keratoacanthoma shares similarities with squamous cell carcinoma, but there are key differences. Unlike squamous cell carcinoma, keratoacanthomas grow quickly but do not invade surrounding tissues. They also have clear boundaries and a classic crater-like structure. The base of the lesion often appears red and inflamed, but the lesion itself remains well-contained. Imaging studies can sometimes help distinguish keratoacanthomas, as they show a thin rim enhancement and no deep tissue invasion. These features, along with a biopsy, help dermatologists confirm the diagnosis and rule out other skin conditions.
Tip: Early evaluation of any suspicious lesion can help ensure proper treatment and prevent complications.
Causes and Risk Factors of Keratoacanthoma
Causes
Role of UV exposure and damage to skin cells
Prolonged exposure to ultraviolet (UV) rays plays a significant role in the development of keratoacanthoma. UV radiation damages the DNA in your skin cells, which can lead to the formation of these tumors. Spending long hours in the sun without protection increases your risk. This is especially true if you live in areas with high sun intensity or frequently engage in outdoor activities.
Other factors, such as trauma or local injuries, can also trigger keratoacanthoma. For example, a surgical procedure or a wound may create conditions that promote tumor growth. Additionally, exposure to chemical carcinogens, such as tar or certain industrial chemicals, has been linked to this condition. Viral infections, particularly with human papillomavirus (HPV), may also contribute. Genetic mutations, including changes in the p53 or H-Ras genes, further increase susceptibility.
Genetic predisposition and other contributing factors
Your genetic makeup can influence your likelihood of developing keratoacanthoma. Mutations in specific genes, such as p53 and H-Ras, are associated with this condition. Some individuals with Muir-Torre syndrome, a rare genetic disorder, experience multiple keratoacanthomas. If you have a family history of skin tumors, you may be at higher risk.
Risk Factors
Older age and male gender
Keratoacanthoma occurs more frequently in older adults, particularly those over 60. The risk increases with age, peaking in individuals aged 70 and above. Men are more likely to develop this condition than women, possibly due to differences in sun exposure habits or hormonal factors.
History of excessive sun exposure or sunburns
If you have a history of frequent sunburns or prolonged sun exposure, your risk of keratoacanthoma rises. Fair-skinned individuals, especially those who burn easily or cannot tan, are particularly vulnerable. Smoking and high alcohol consumption may also contribute to the risk.
Weakened immune system or certain medical conditions
A weakened immune system can make you more susceptible to keratoacanthoma. Conditions like AIDS, cancer treatments, or the use of immunosuppressant drugs can impair your body’s ability to fight abnormal cell growth. If you are immunocompromised, you should monitor your skin closely for any unusual changes.
Note: Protecting your skin from UV rays and maintaining a healthy immune system can help reduce your risk of keratoacanthoma.
Diagnosis of Keratoacanthoma
Medical Evaluation
Physical examination and patient history
Diagnosing keratoacanthoma begins with a thorough medical evaluation. Your doctor will examine the lesion visually and ask about your medical history, including any history of sun exposure or skin conditions. They may use tools like dermoscopy, which magnifies the lesion to reveal specific patterns. In some cases, a Wood’s lamp examination, which uses ultraviolet light, helps identify pigmentation changes. These steps allow the doctor to gather essential details about the lesion's appearance and behavior.
Identifying lesion characteristics
Keratoacanthomas typically go through three stages: proliferation, stabilization, and regression. During the proliferation stage, the lesion grows rapidly into a dome-shaped nodule with a central depression. The stabilization stage involves a pause in growth, while the regression stage may lead to spontaneous resolution. These characteristics, along with the lesion's location on sun-exposed areas like the face or hands, help your doctor identify it.
Diagnostic Tests
Skin biopsy to confirm the diagnosis
A skin biopsy is the gold standard for confirming keratoacanthoma. If your lesion resembles squamous cell carcinoma, your doctor will remove a small sample or the entire lesion under local anesthesia. This sample is sent to a lab for microscopic examination. The biopsy often reveals keratin-filled fragments and other features unique to keratoacanthoma. This test ensures an accurate diagnosis and rules out more serious conditions.
Differential Diagnosis
Distinguishing keratoacanthoma from squamous cell carcinoma and other skin tumors
Keratoacanthoma shares similarities with squamous cell carcinoma, making differentiation challenging. However, key differences exist. For example, keratoacanthomas grow rapidly but often resolve on their own, while squamous cell carcinoma progresses continuously. Histological analysis from a biopsy reveals keratoacanthoma's dome-shaped structure and keratin-filled crater, unlike the invasive nature of squamous cell carcinoma. The table below highlights additional distinctions:
Feature | Keratoacanthoma | Squamous Cell Carcinoma |
|---|---|---|
Clinical Behavior | Self-healing, rapid onset | Malignant, continuous progression |
Histological Features | Dome-shaped keratin-filled crater | Cellular atypia, stromal invasion |
Spontaneous Resolution | Yes | No |
Tip: Early diagnosis and biopsy are crucial to distinguish keratoacanthoma from other skin tumors and ensure proper treatment.
Treatment Options for Keratoacanthoma

Surgical Treatments
Excision to remove the lesion completely
Surgical excision is the most common treatment for keratoacanthoma. Your doctor will remove the lesion along with a margin of healthy tissue (3-5 mm) to ensure complete removal. This approach also allows for histopathologic evaluation to rule out invasive squamous cell carcinoma. While keratoacanthomas may resolve on their own, excision is often recommended to avoid complications.
Most keratoacanthomas are treated surgically. Although they may resolve spontaneously, it is usually prudent to excise them, unless there is clear evidence that regression is in progress.
Mohs surgery for precise removal and minimal scarring
For larger or recurrent keratoacanthomas, Mohs surgery offers a highly effective option. This technique removes the tumor layer by layer while preserving as much healthy tissue as possible. It minimizes scarring and ensures complete removal of cancerous cells.
Mohs surgery preserves healthy tissue by excising cancerous cells layer by layer, minimizing the removal of surrounding healthy skin.
Utilizing real-time microscopy enhances accuracy, leading to effective treatment with less trauma to the patient.
Non-Surgical Treatments
Topical or injectable medications
Non-surgical options include antineoplastic agents like 5-fluorouracil and methotrexate. These can be applied topically or injected directly into the lesion. Topical imiquimod and systemic retinoids, such as isotretinoin, are also used for patients with multiple lesions or those unsuitable for surgery.
Antineoplastic agents such as topical and intralesional 5-fluorouracil, intralesional methotrexate, and topical imiquimod have shown success in treating keratoacanthomas.
Cryotherapy or laser therapy for smaller lesions
Cryotherapy and laser therapy are effective for smaller keratoacanthomas. Cryotherapy involves freezing the lesion, while laser therapy uses focused light to destroy abnormal cells. Both methods offer excellent cosmetic outcomes with minimal adverse effects.
Treatment Method | Success Rate | Adverse Events | Cosmetic Outcome |
|---|---|---|---|
Cryotherapy + Curettage + Electrodessication | None reported | Excellent |
Post-Treatment Care
Wound care and monitoring for recurrence
After treatment, proper wound care helps prevent infection and promotes healing. You should monitor the treated area for any signs of recurrence. Protecting your skin from UV exposure is crucial to reduce the risk of new lesions.
Avoid UV light exposure from natural sunlight and artificial tanning devices.
Wear broad-spectrum sunscreens (SPF 30 or higher) and reapply frequently.
Wear wide-brimmed hats and long-sleeved shirts.
Regular follow-up visits with a dermatologist
Frequent follow-up appointments with your dermatologist are essential. These visits help ensure the keratoacanthoma has not returned and allow for early detection of any new skin cancers. Regular monitoring is a key step in maintaining healthy skin.
After the removal of keratoacanthoma, it is crucial to have regular follow-up appointments with a dermatologist to monitor for any recurrence of the condition or the emergence of new skin cancers.
Prevention and Prognosis of Keratoacanthoma
Prevention Strategies
Use of sunscreen and protective clothing
Protecting your skin from harmful UV rays is one of the most effective ways to prevent keratoacanthoma. Use a broad-spectrum sunscreen with an SPF of 30 or higher whenever you go outdoors. Reapply it every two hours, especially if you are swimming or sweating. Wearing protective clothing, such as long-sleeved shirts, wide-brimmed hats, and sunglasses, can also shield your skin from sun damage. These measures reduce the risk of developing keratoacanthoma and other sun-related skin conditions.
Avoiding peak sun hours and practicing sun safety
Avoid staying outdoors during peak sun hours, typically between 10 a.m. and 4 p.m., when UV rays are strongest. If you must be outside, seek shade whenever possible. Avoid artificial UV sources like tanning beds, as they can increase your risk of skin damage. Regularly check your skin for new or unusual growths. If you notice any changes, consult a dermatologist promptly. Early action can make a significant difference in preventing complications.
Tip: Make sun protection a daily habit to safeguard your skin and reduce the risk of keratoacanthoma.
Prognosis
High success rate with treatment
The prognosis for keratoacanthoma is excellent, especially when treated early. Surgical removal, such as excision or Mohs surgery, often leads to complete resolution. Studies show that less than 20% of cases experience complications or recurrence after treatment. However, untreated lesions may progress or mimic more serious conditions like squamous cell carcinoma. Regular follow-ups with your dermatologist ensure that any new or recurring lesions are addressed promptly.
Source | Evidence |
|---|---|
eMedicine | The prognosis for keratoacanthoma is excellent following excisional surgery. |
DermNet NZ | Keratoacanthoma is benign with an excellent prognosis post-surgery. |
News Medical | The prognosis is excellent after surgery, with less than a 20% chance of spreading. |
Importance of early detection to prevent complications
Detecting keratoacanthoma early ensures better outcomes. Early intervention allows for complete removal of the lesion, minimizing the risk of complications. If left untreated, the lesion may grow larger or cause scarring. Regular skin checks and prompt medical attention for suspicious growths can help you maintain healthy skin and avoid unnecessary risks.
Note: Early detection and treatment not only improve the prognosis but also reduce the likelihood of scarring or recurrence.
Keratoacanthoma often appears alarming due to its rapid growth, but it is usually benign and treatable. Early detection allows for effective treatment, such as surgical removal, which ensures an excellent prognosis. You can feel reassured knowing that most cases resolve without complications when addressed promptly. If you notice any unusual skin lesions, consulting a dermatologist is essential. Regular skin checks and sun protection can help you maintain healthy skin and prevent future issues.
FAQ
What should you do if you notice a rapidly growing skin lesion?
You should consult a dermatologist immediately. Rapidly growing lesions may resemble keratoacanthoma or other serious conditions. Early evaluation ensures accurate diagnosis and timely treatment, reducing the risk of complications.
Tip: Always monitor your skin for unusual changes and seek medical advice promptly.
Can keratoacanthoma resolve without treatment?
Yes, keratoacanthoma can sometimes regress spontaneously. However, you should not rely on this. Untreated lesions may grow larger or mimic more serious conditions like squamous cell carcinoma. A dermatologist can guide you on the best course of action.
Is keratoacanthoma contagious?
No, keratoacanthoma is not contagious. It develops due to factors like UV damage, genetics, or a weakened immune system. You cannot spread it to others through physical contact.
How can you differentiate keratoacanthoma from squamous cell carcinoma?
A biopsy is the most reliable way to differentiate the two. Keratoacanthoma grows rapidly but often resolves, while squamous cell carcinoma progresses continuously. Both conditions may look similar, so professional evaluation is essential.
Does sunscreen help prevent keratoacanthoma?
Yes, sunscreen reduces your risk by protecting your skin from harmful UV rays. Use a broad-spectrum sunscreen with SPF 30 or higher. Reapply it every two hours when outdoors, especially during peak sun hours.
Note: Combine sunscreen with protective clothing for maximum sun safety.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Exploring Craniopharyngioma: Key Features and Insights
Cholangiocarcinoma Explained: Essential Traits and Information
Conjunctival Melanoma: Recognizing Symptoms and Treatment Options
Hemangioblastoma: A Comprehensive Overview of Its Characteristics

