Understanding Medulloblastoma and Its Causes
Medulloblastoma is a fast-growing, cancerous tumor that develops in the cerebellum, the part of your brain responsible for balance and coordination. This type of brain tumor primarily affects children, especially those aged 5 to 9. It is rare in adults, accounting for less than 1% of adult brain tumors.
You should know that medulloblastoma can spread to other parts of the brain and spinal cord. About one-third of cases show this type of spread, which makes early detection crucial. Scientists believe its causes include genetic mutations, inherited syndromes, and developmental factors that affect brain growth.
Key Takeaways
Medulloblastoma is a fast-growing brain tumor in kids aged 5 to 9. Finding it early helps with better treatment results.
Genetic causes, like inherited conditions or sudden gene changes, raise the chance of getting medulloblastoma.
Common signs include headaches, feeling sick, and trouble balancing. Spotting these signs early helps with quick diagnosis and care.
New genetic studies help create treatments that match each tumor's traits.
Current medical tests are finding new treatments and lowering side effects of older ones, making life better for patients.
What Is Medulloblastoma?
Characteristics of Medulloblastoma
Location in the cerebellum and proximity to the brainstem
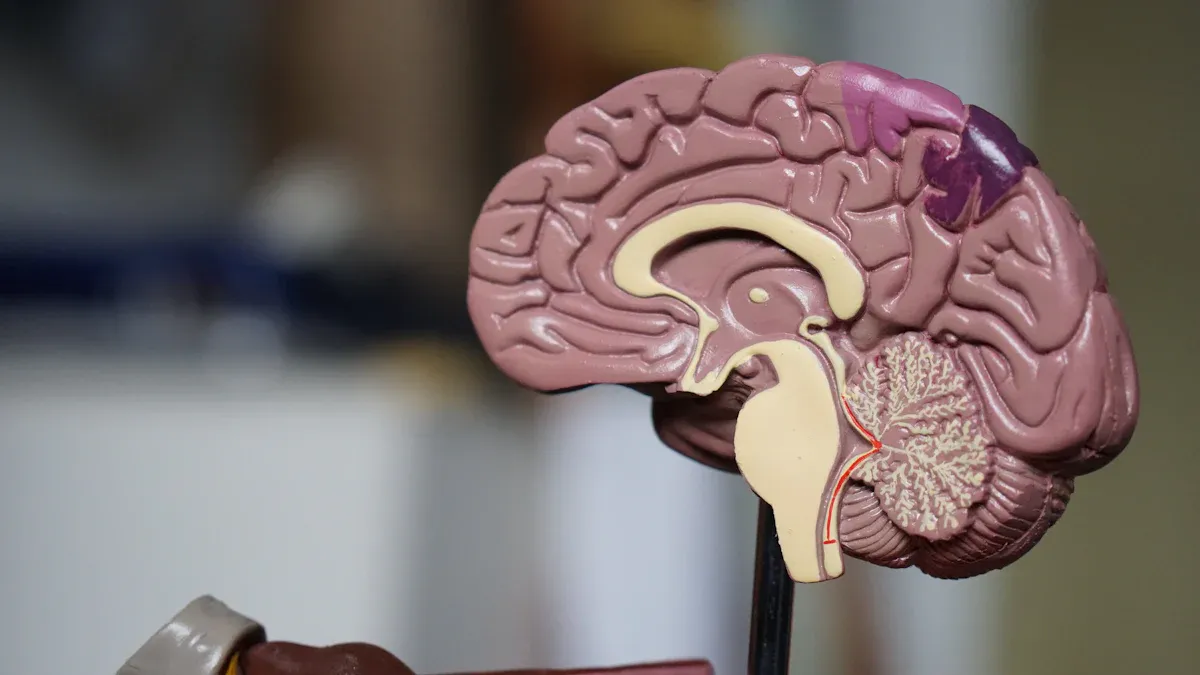
Medulloblastoma develops in the cerebellum, the part of your brain that controls balance, coordination, and fine motor skills. This tumor often grows near the brainstem, which connects your brain to the spinal cord. Its location can lead to symptoms that affect movement and coordination. Medulloblastomas are classified as grade 4 tumors, meaning they grow quickly and are malignant. This aggressive nature sets them apart from many other brain tumors, which may grow more slowly or be less harmful.
Medulloblastomas are also unique because they are divided into four molecular subgroups. These include the WNT subtype (10% of cases), SHH subtype (30%), Group 3 (25%), and Group 4 (35%). This classification helps doctors predict outcomes and choose the best treatment for you.
How it spreads to other parts of the brain and spinal cord
Medulloblastoma can spread through cerebrospinal fluid, the liquid surrounding your brain and spinal cord. This spread, called metastasis, often affects other areas of the brain or spinal cord. When this happens, you may experience additional symptoms like back pain, difficulty walking, or changes in bowel and bladder function. Early detection is crucial to prevent the tumor from spreading further.
Symptoms and Diagnosis
Common symptoms
You might notice symptoms like headaches, nausea, or vomiting, especially in the morning. These symptoms often improve after vomiting. Other signs include dizziness, tiredness, and changes in activity levels. You may also experience balance problems, clumsiness, or difficulty with handwriting. If the tumor spreads to your spinal cord, you could have back pain, trouble walking, or issues with urination and bowel movements.
Diagnostic methods
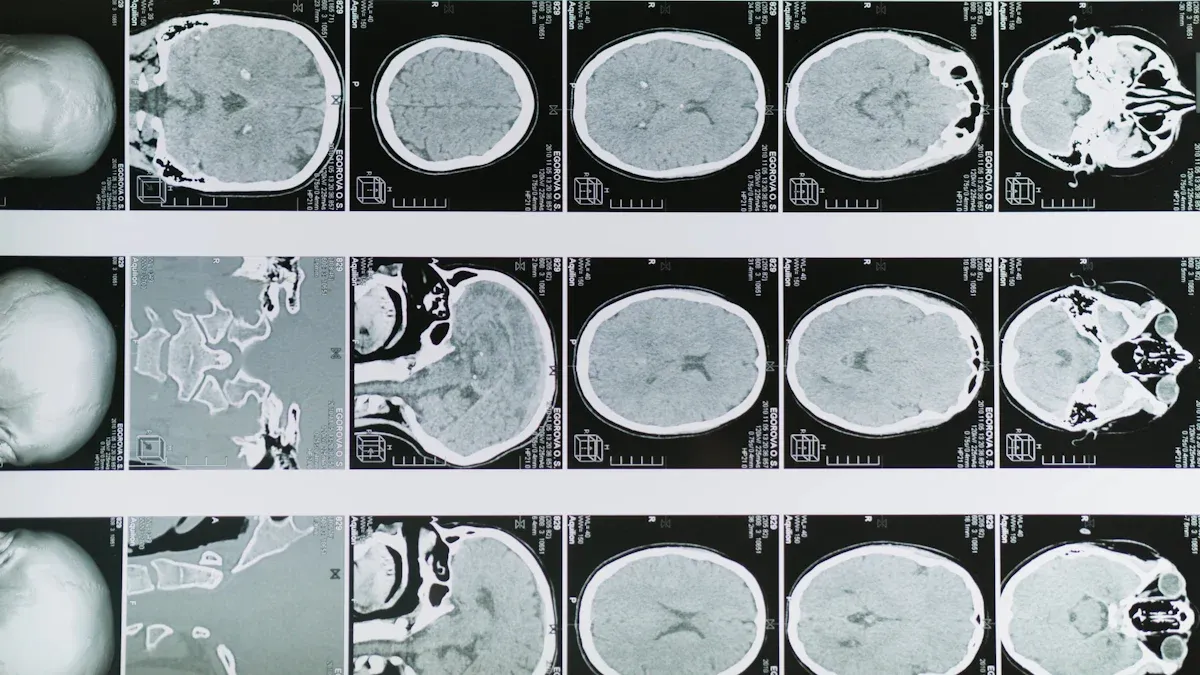
Doctors use imaging techniques like Magnetic Resonance Imaging (MRI) to diagnose medulloblastoma. MRI provides detailed images of your brain and can identify the tumor's size, location, and characteristics. It is the most effective tool for detecting medulloblastoma and monitoring its progression. In some cases, a biopsy may be performed to confirm the diagnosis and determine the tumor's molecular subgroup.
What Causes Medulloblastoma?
Genetic Factors
Inherited syndromes (e.g., Gorlin syndrome, Li-Fraumeni syndrome)
Certain inherited syndromes increase your risk of developing medulloblastoma. For example, Gorlin syndrome, also called Nevoid Basal Cell Carcinoma Syndrome, results from mutations in the PTCH1 gene. These mutations disrupt the SHH (Sonic Hedgehog) signaling pathway, which plays a key role in brain development. Similarly, Li-Fraumeni syndrome, caused by mutations in the TP53 gene, raises your overall cancer risk, including brain tumors like medulloblastoma. Another condition, Turcot syndrome, involves mutations that impair DNA repair, making you more vulnerable to brain tumors.
Spontaneous genetic mutations during brain development
Many cases of medulloblastoma arise from genetic mutations that occur spontaneously during brain development. These mutations lead to uncontrolled cell growth in the cerebellum, resulting in tumor formation. Unlike inherited syndromes, these changes are not passed down from parents but happen randomly as the brain develops.
Molecular subgroups and their significance
Medulloblastoma is divided into four molecular subgroups: WNT, SHH, Group 3, and Group 4. Each subgroup has unique genetic traits that influence treatment and outcomes. For instance, the WNT subtype, which accounts for 10% of cases, generally has a better prognosis. The SHH subtype, linked to specific genetic pathways, represents 30% of cases. Group 3 and Group 4, which make up 25% and 35% of cases respectively, have distinct genetic features that affect how the tumor behaves and responds to treatment.
Developmental Influences
Prenatal factors affecting brain development
Your brain's development before birth can influence the risk of medulloblastoma. Exposure to harmful substances or infections during pregnancy may disrupt normal brain growth, increasing the likelihood of tumor formation.
Other developmental abnormalities
Abnormalities in brain development, such as issues with cell division or migration, can also contribute to medulloblastoma. These disruptions may create an environment where cells grow uncontrollably, leading to tumor formation.
Environmental Factors
Limited evidence on radiation exposure
Radiation exposure is a recognized risk factor for brain tumors. If you underwent radiation therapy as a child for another condition, your risk of developing secondary tumors, including medulloblastoma, might slightly increase.
Unconfirmed links to toxins or chemicals
Some studies suggest that parental exposure to chemicals like pesticides or industrial toxins could play a role in medulloblastoma. However, these findings remain inconclusive, and no specific environmental cause has been definitively linked to this tumor.
Who Is Affected by Medulloblastoma?
Age Groups
Predominance in children under 16
Medulloblastoma primarily affects children and teenagers. About 70% of cases occur in individuals under the age of 16, with most diagnoses happening between the ages of 4 and 9. You might notice that this tumor is more common during early childhood, a period when the brain undergoes rapid development.
Rare occurrence in adults
Although medulloblastoma is rare in adults, it can still occur. When it does, the tumor often presents differently compared to children.
Aspect | Children | Adults |
|---|---|---|
Tumor Location | More likely to be midline | More likely to be lateralized |
Histology | Lower rates of desmoplastic histology | Higher rates of desmoplastic histology |
Molecular Subtypes | More diverse subtypes | Group C tumors are more rare |
Treatment Approaches | Standardized protocols exist | Uncertainty in treatment similarity to children |
This table highlights key differences in how medulloblastoma manifests across age groups. These variations can influence treatment decisions and outcomes.
Demographics and Risk Factors
Slightly higher prevalence in males
Medulloblastoma occurs slightly more often in males than females.
Gender | Incidence of Medulloblastoma |
|---|---|
Male | Higher |
Female | Lower |
Researchers believe this difference may result from genetic or hormonal factors, though the exact reasons remain unclear.
Geographic and environmental trends
Geographic trends suggest that medulloblastoma occurs worldwide, but its incidence varies slightly by region. Environmental factors, such as exposure to industrial toxins or pesticides, have been studied, but no definitive links have been established. You should know that these trends are still under investigation, and more research is needed to understand their significance.
Ongoing Research and Treatment Advances
Genomic Studies
Identifying genetic mutations and molecular pathways
Recent genomic studies have uncovered new genetic mutations linked to medulloblastoma. Two genes, KBTBD4 and PRDM6, have been identified as key players in Group 3 and Group 4 subtypes. KBTBD4 mutations occur most frequently in these subgroups, while PRDM6 activation contributes to 17% of Group 4 tumors. These discoveries enhance your understanding of how genetic alterations drive tumor growth and pave the way for more targeted therapies.
Implications for personalized medicine
Genomic research has revealed that over 75% of medulloblastoma cases involve specific genetic changes. This knowledge supports the development of personalized medicine, where treatments are tailored to the unique molecular characteristics of each tumor.
Evidence | Description |
|---|---|
Genomic Alterations | Identified genetic changes responsible for most cases, including new cancer genes. |
Precision Medicine | Enables targeted therapies to improve survival and reduce side effects. |
Molecular Understanding | Highlights the importance of molecular-level insights for customized treatments. |
Personalized approaches, such as patient-derived tumor models, help identify effective drugs for individual patients. These methods go beyond traditional sequencing, offering more options for treatment.
Targeted Therapies
Immunotherapy and precision medicine
Immunotherapy is emerging as a promising treatment for medulloblastoma. Researchers are testing strategies like CAR-T cells, RNA vaccines, and adoptive natural killer (NK) cells to target tumor cells. A trial combining precision adoptive T-cell therapy with PD-1 inhibitors aims to enhance the immune system's ability to fight cancer.
Reducing side effects of traditional treatments
Efforts to reduce the side effects of radiation and chemotherapy focus on less aggressive subgroups like WNT-driven medulloblastoma. Lowering treatment doses minimizes long-term issues, such as learning difficulties and hormonal imbalances. Additionally, the FDA recently approved sodium thiosulfate to prevent hearing loss in children receiving cisplatin. This drug is administered intravenously after chemotherapy to protect hearing without compromising treatment effectiveness.
Clinical Trials and Innovations
Current trials for new drugs and therapies
Several clinical trials are exploring innovative treatments for medulloblastoma. Researchers at the University of Florida are leading the first human trials for Group 4 medulloblastoma. Other trials include:
PLX038 in CNS Tumors: Investigating a new drug for central nervous system tumors.
Nivolumab for Rare CNS Cancers: Testing an immune checkpoint inhibitor for rare brain cancers.
ONC206 for Rare CNS Neoplasms: Assessing a novel therapy for rare brain tumors, including medulloblastoma.
Collaboration between research institutions
Global collaborations drive progress in medulloblastoma research. The Medulloblastoma Working Group, comprising scientists, physicians, and advocates, meets monthly to share findings and discuss therapies. Another initiative, the Medulloblastoma Special Interest Group, focuses on creating preclinical models for specific subgroups and improving drug delivery to the brain. These partnerships accelerate innovation and improve outcomes for patients like you.
Understanding medulloblastoma begins with recognizing its causes. Genetic factors, including inherited conditions like Gorlin and Li-Fraumeni syndromes, play a significant role. Spontaneous mutations and molecular subgroups also influence tumor behavior and treatment outcomes. Researchers continue to explore environmental links and develop targeted therapies to improve survival rates.
Early diagnosis remains critical. Identifying symptoms and understanding risk factors can lead to timely treatment, which is essential for better outcomes. Advances in molecular diagnostics now allow doctors to classify medulloblastoma into four subgroups, enabling personalized treatment plans. Clinical trials are also testing reduced radiation and chemotherapy doses for less aggressive cases, aiming to improve quality of life.
Ongoing research offers hope. With innovations in diagnostics and therapies, the future looks brighter for those affected by this condition.
FAQ
What is the survival rate for medulloblastoma?
The survival rate depends on factors like age, tumor subtype, and treatment. For children, it ranges from 70% to 85% for standard-risk cases. High-risk cases have lower survival rates. Early diagnosis and advanced treatments improve outcomes.
Can medulloblastoma recur after treatment?
Yes, medulloblastoma can recur, especially in high-risk cases. Recurrence often happens within two years of treatment. Regular follow-ups and imaging help detect any signs of recurrence early.
Are there long-term side effects of medulloblastoma treatment?
Treatments like radiation and chemotherapy may cause long-term effects. These include learning difficulties, hormonal imbalances, or hearing loss. Advances in therapy aim to reduce these side effects while maintaining effectiveness.
Is medulloblastoma hereditary?
Most cases are not hereditary. However, certain genetic syndromes, like Gorlin or Li-Fraumeni, increase your risk. Genetic counseling can help assess your family’s risk if these syndromes are present.
How can I support a loved one with medulloblastoma?
Offer emotional support and help with daily tasks. Encourage them to attend medical appointments and follow treatment plans. Joining support groups can also provide valuable resources and connections.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Key Characteristics of Glioblastoma You Should Know
A Comprehensive Guide to Different Types of Blastoma
Simplifying B-Cell Prolymphocytic Leukemia for Better Understanding

