Cancer Vaccines in 2025 What’s New

You see exciting changes in cancer vaccine development in 2025. mRNA vaccines now use better structures and lipid nanoparticles, making them more stable and easier to deliver. These advances help scientists design vaccines quickly and target cancer cells more effectively. You benefit from safer options, since mRNA vaccines do not change your DNA. Researchers focus on personalized vaccines and adjuvant therapies to improve results. The table below shows important trends in this field, giving you updates on Cancer Vaccines: Progress and Perspectives.
Trend Description | Details |
|---|---|
Ongoing Clinical Trials | Many trials are testing vaccines against mutation-derived antigens across various cancers. |
Focus on Adjuvant Therapies | Vaccines are primarily being used for secondary prevention after primary cancer removal. |
Exploration of Vaccine Types | There is interest in personalized vaccines versus off-the-shelf vaccines for shared antigens. |
Key Takeaways
mRNA vaccines are safer and more effective, as they do not alter your DNA and can be tailored to target specific cancer cells.
Personalized cancer vaccines are on the rise, allowing treatments to be designed based on the unique features of your tumor.
New delivery methods, like lipid nanoparticles, enhance the effectiveness of vaccines by ensuring they reach the right cells in your body.
Recent trials show promising results, with many patients experiencing longer periods without cancer recurrence after receiving these vaccines.
Ongoing research aims to improve vaccine technology and combine treatments, offering hope for more effective cancer care in the future.
Key Breakthroughs
Vaccine Platforms
You now see a new era in cancer vaccine platforms. Scientists have made big progress with RNA-based vaccines and virus-like particle (VLP) vaccines. These new platforms help you fight cancer more effectively.
Cancer prevention vaccines, like those for HPV and hepatitis B, have already lowered cancer rates by stopping virus-related cancers.
Therapeutic cancer vaccines faced many challenges in the past. Now, you benefit from new hope as these vaccines show better results in trials.
Personalized mRNA vaccines are changing the way you receive cancer treatment. In 2023, a small trial for pancreatic cancer used mRNA vaccines and showed positive results. This means you could get a vaccine designed just for your tumor.
The first mRNA neoantigen vaccine, XH101, received approval for clinical testing in China in 2023. This step brings you closer to more treatment options.
In 2024, a new vaccine called Gnos-PV02, when combined with a PD-1 inhibitor, helped patients with advanced liver cancer.
The UK’s NHS started a large study in 2024 to test personalized cancer vaccines for many patients.
You also see new ways to target cancer. Modern vaccines focus on tumor-specific antigens, called neoantigens. These targets help your immune system find and attack cancer cells more precisely. Advances in tumor profiling and vaccine design make these vaccines stronger and more specific.
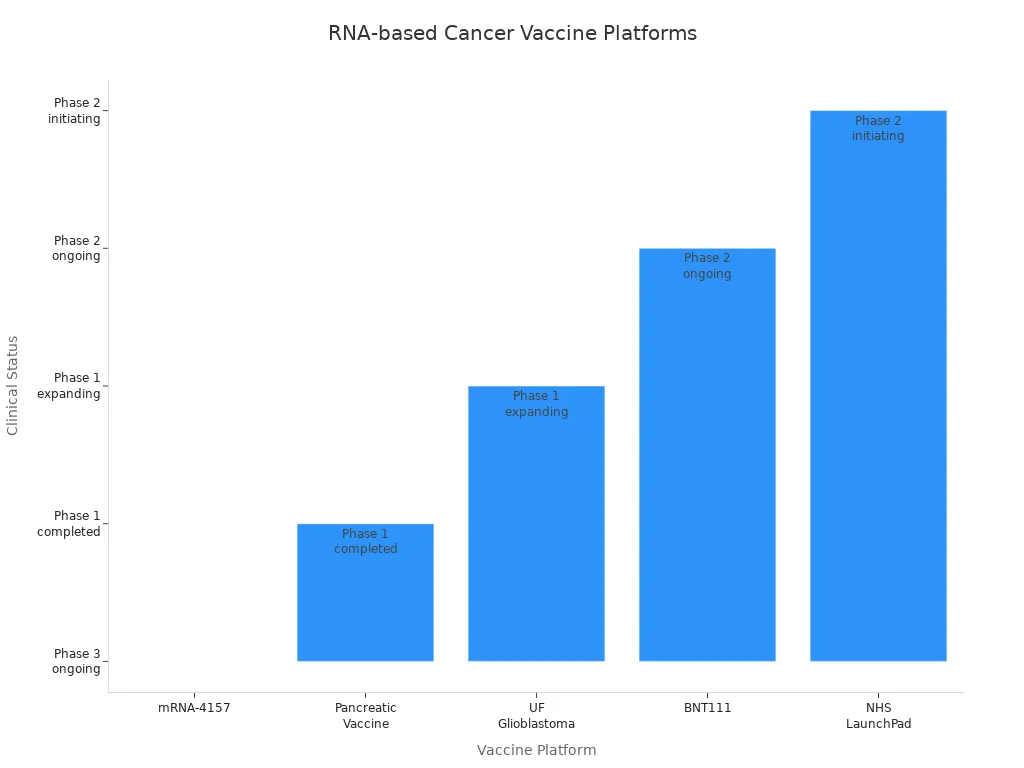
Here is a table showing some of the most promising RNA-based and VLP vaccine platforms:
Vaccine | Cancer Type | Platform | Key Results | Clinical Status |
|---|---|---|---|---|
mRNA-4157 | Melanoma | Personalized mRNA | 44% lower recurrence risk; 3-year benefit | Phase 3 ongoing |
Pancreatic Vaccine | PDAC | Personalized mRNA | 4-year immune response; less recurrence | Phase 1 completed |
UF Glioblastoma | Brain Cancer | Layered nanoparticle mRNA | 48-hour immune activation; 4x survival in dogs | Phase 1 expanding |
BNT111 | Melanoma | Fixed antigen mRNA | Better response than past treatments | Phase 2 ongoing |
NHS LaunchPad | Multiple | Personalized mRNA | Thousands enrolled in screening | Phase 2 starting |
You can also look at the chart below to compare the progress of different RNA-based vaccine platforms:
New platform types bring more benefits:
Platform Type | Key Innovation | Advantages | Clinical Stage | Applications |
|---|---|---|---|---|
Layered Nanoparticles | Multi-layer fat coating, high mRNA | Fast immune activation (<48 h) | Phase 1 | Glioblastoma, solid tumors |
Circular RNA | Closed loop structure | More stable, easy storage | Preclinical | Many cancer types |
Self-Amplifying | Viral replication machinery | Lower doses, longer effect | Phase 1/2 | Liver cancer |
CRISPR-Enhanced | Gene editing integration | Better immune targeting | Early preclinical | Personalized vaccines |
Nanoengineered | Targeted delivery systems | Tumor-specific delivery | Preclinical/Phase 1 | Solid tumors |
Delivery Methods
You benefit from new delivery methods that make cancer vaccines safer and more effective. RNA-based vaccines use lipid nanoparticles (LNPs) to carry the vaccine into your cells. This method helps protect the mRNA and delivers it where it is needed.
RNA-based vaccines can be made quickly and tailored for you. This means you get a treatment that matches your cancer’s unique features.
Lipid nanoparticles are the main delivery tool, but they can have problems with stability and storage. Scientists are working on new systems to improve targeting and reduce side effects.
Neoantigen vaccines come in different forms. You might receive a peptide-based, nucleic acid-based, or dendritic cell-based vaccine.
Dendritic cell vaccines use your own immune cells. These vaccines are stable and can trigger strong immune responses.
Tip: Personalized delivery methods help your immune system recognize and attack cancer cells more accurately.
Immune Response
You want a vaccine that gives you a strong and safe immune response. mRNA cancer vaccines do just that. They use your body’s own cells to make proteins that teach your immune system to find and destroy cancer.
mRNA vaccines create a reliable immune response and are well-tolerated. You do not face the risks linked to vaccines that use live viruses.
These vaccines can be made quickly and at a lower cost. You do not have to wait long for new treatments.
mRNA vaccines can show your immune system many parts of the cancer cell, which helps your body attack the cancer from different angles.
You get a stronger T cell response, which is important for fighting cancer.
The immune response from mRNA vaccines looks like the response to a real viral infection. This means your body learns to fight cancer more effectively.
mRNA vaccines use your cells to make special proteins, so you avoid the risks of live virus vaccines.
You benefit from fast production, which means you get treatment sooner.
mRNA vaccines can show your immune system many targets, not just one, making them more powerful than older vaccines.
You also see better results when mRNA vaccines are combined with immune checkpoint inhibitors. Patients with melanoma and kidney cancer who received these combinations had longer periods without cancer coming back. In pancreatic cancer, patients who responded to a personalized mRNA vaccine had longer times before the cancer returned.
Note: These breakthroughs mean you have more hope for effective, safe, and fast cancer treatments in 2025.
Clinical Updates
Trial Results
You see many new results from cancer vaccine trials in 2025. These results show real progress in fighting cancer with vaccines. Here are some of the most notable findings:
A phase 1 study on a new breast cancer vaccine showed that over 70% of participants had the expected immune responses. This result gives hope for people with triple negative breast cancer.
A vaccine that targets KRAS mutations in pancreatic and colorectal cancers proved safe. About two-thirds of patients showed strong immune responses. Patients with higher T cell responses lived longer without their cancer coming back.
The vaccine helped activate and grow cancer-fighting T cells. Patients who had more of these T cells enjoyed longer periods without relapse.
These results mean you can expect more effective and safer cancer vaccines in the near future. You benefit from treatments that not only target your cancer but also help your immune system remember how to fight it.
Cancer Types
You now see cancer vaccines being tested for more types of cancer than ever before. In 2025, researchers focus on both common and rare cancers. The table below shows some of the main cancer types and the focus of current vaccine trials:
Cancer Type | Trial Focus |
|---|---|
Pancreatic Cancer | mRNA vaccine trials aim to reduce tumor growth and prevent recurrence. |
Nonsmall Cell Lung Cancer | mRNA vaccine trials aim to reduce tumor growth and prevent recurrence. |
In 2025, you find that vaccine trials use mRNA technology to create personalized vaccines. These vaccines train your immune system to recognize cancer-specific antigens. This approach helps reduce tumor growth and lowers the chance of cancer coming back.
A phase I clinical trial now tests an mRNA vaccine in patients with pancreatic ductal adenocarcinoma (PDAC). Doctors create these vaccines based on the unique antigens found in each patient’s tumor. This means you could receive a vaccine designed just for your cancer.
The range of cancers addressed by vaccine research has grown. In the United States, over 20 cancer types are part of vaccine clinical trials. Top cancer types include breast cancer, cervical cancer, lung cancer, melanoma, and pancreatic cancer. This broad scope gives you more options and hope for new treatments.
Safety Data
You want to know if cancer vaccines are safe. Recent trials show that most side effects are mild or moderate. The tables below list the most common adverse events and their severity:
Adverse Event | Severity Level |
|---|---|
Injection site reaction | Mild |
Injection site hematoma | Mild |
Peripheral edema | Mild |
Chills | Mild |
Myalgia | Mild |
Back pain | Mild |
Lymphadenopathy | Mild |
Moderate injection site reaction | Moderate |
No grade 3 or 4 toxicities | N/A |
Adverse Event | Severity Level |
|---|---|
Fatigue | Grade 2 |
Decreased white blood cell count | Grade 2 |
Diarrhea | Grade 1 |
Rash | Grade 1 |
Oral mucositis | Grade 1 |
Malaise | Grade 1 |
Nausea | Grade 1 |
Dry mouth | Grade 1 |
Sore throat | Grade 1 |
Decreased neutrophil count | Grade 1 |
No grade 3 or 4 toxicities | N/A |
You see that most people experience only mild reactions, such as soreness at the injection site, chills, or mild fatigue. No grade 3 or 4 toxicities have been reported in recent trials. This means you can feel confident that cancer vaccines are becoming safer as research advances.
Note: You benefit from vaccines that not only target your cancer but also come with a low risk of serious side effects. Researchers continue to monitor safety closely in every trial.
Updates on Cancer Vaccines: Progress and Perspectives
Regulatory Approvals
You see more cancer vaccines moving closer to approval in 2025. Health agencies in the United States, Europe, and Asia now review new vaccine data faster. Some mRNA vaccines for melanoma and pancreatic cancer have entered late-stage trials. You may soon have access to these vaccines if they meet safety and effectiveness standards. The Updates on Cancer Vaccines: Progress and Perspectives show that more countries are preparing to approve these treatments for wider use.
Market Access
Getting cancer vaccines to you involves more than just approval. Health systems must decide how to pay for these new treatments. You may notice that some vaccines cost more, especially when used with other therapies. The Updates on Cancer Vaccines: Progress and Perspectives highlight several barriers to market access:
Barrier Description | Details |
|---|---|
Clinical Efficacy Challenges | Proving that vaccines work well, especially in early-stage cancer, remains difficult. |
High Costs of Combination Therapies | Using vaccines with other drugs can raise costs, making approval harder. |
Complex Reimbursement Models | Insurance companies want long-term survival data, which takes time to collect. |
To help you, healthcare systems use special reviews called Health Technology Assessments. These reviews look at both the health benefits and the costs. You also see more groups working together, including doctors and patient advocates, to make vaccines easier to get.
Challenges
You face some challenges with cancer vaccines. Tumors can hide from your immune system, making vaccines less effective. Solid tumors are especially hard to treat. Making personalized vaccines costs a lot, and doctors must choose the right patients for each treatment. The Updates on Cancer Vaccines: Progress and Perspectives point to new opportunities:
Opportunity Type | Description |
|---|---|
Advancements in Adjuvants | New ingredients boost vaccine power and are already helping some patients. |
Delivery Technologies | Better ways to deliver vaccines protect them and help them reach cancer cells. |
Combination Therapies | Using vaccines with other treatments can help your immune system fight cancer more strongly. |
Tip: Stay informed about Updates on Cancer Vaccines: Progress and Perspectives. New research and teamwork between experts give you more hope for better treatments.
Patient Impact

Outcomes
You see real changes in patient outcomes as new cancer vaccines reach clinics. Many people now experience longer periods without cancer returning. Some even see their tumors shrink or disappear. The table below highlights recent results from different vaccine combinations:
Vaccine/Combination | Patient Population | Outcome | Notes |
|---|---|---|---|
mRNA-4157 + Pembrolizumab | High-risk melanoma | 44% lower risk of disease progression or death | Breakthrough Therapy designation |
EO2401 + Nivolumab | Recurrent brain cancer (GBM) | Improved response and longer time without relapse | More cancer-fighting T cells |
IO102/IO103 + Pembrolizumab | Lung adenocarcinoma (high PD-L1) | 53.3% had tumor shrinkage, 26.7% stable disease | Early clinical activity |
GRANITE (GRT-C901/GRT-R902) | Colorectal cancer (MSS-CRC) | 18% lower risk of progression or death | Median time without progression: 11.57 months |
GNOS-PV02 + PD-1 inhibitor | Advanced liver cancer (HCC) | 30.6% response rate (3 complete, 8 partial) | Better than standard treatment |
You benefit from these advances because doctors can now offer more options and hope for better results.
Research Directions
You see researchers focus on making vaccines more personal and effective. They test new vaccines in kidney cancer, where all patients in one study stayed cancer-free for almost three years after surgery. Doctors gave the vaccine soon after removing the tumor, and patients’ immune systems responded quickly and strongly.
Ongoing research explores several promising directions:
Personalized vaccines that match your tumor’s unique features
Use in many cancer types, especially kidney cancer
New ways to boost your immune response for lasting protection
Larger studies to confirm early success and combine vaccines with other treatments
Scientists also work on understanding the tumor microenvironment and how to overcome barriers that stop the immune system from working well. You may soon see vaccines that work better by combining them with other therapies.
Expert Views
Experts believe the future of cancer vaccines looks bright. Dr. Nina Bhardwaj explains that personalized vaccines for melanoma show great promise, especially when combined with checkpoint inhibitors like pembrolizumab. These combinations help more patients stay cancer-free for longer.
Many experts highlight new technologies, such as DNA-based vaccines, nanoparticle delivery, and CRISPR gene editing. They see these tools as ways to make vaccines safer and more powerful. The Updates on Cancer Vaccines: Progress and Perspectives suggest that combining vaccines with other treatments will help you get the best results.
You can expect more breakthroughs as research continues and experts work together to improve cancer care.
You now see cancer vaccines changing how doctors treat cancer. New mRNA vaccines train your immune system to attack cancer cells. Dendritic cell vaccines help your body remember cancer and stop it from coming back. You benefit from therapies that match your tumor and work with other drugs.
Over 120 trials test these vaccines for many cancers.
Patients live longer and have fewer relapses.
Future research will bring more targeted and powerful treatments.
Key Area | Description |
|---|---|
Next gen immunotherapy | Stacking therapies like engineered cells and vaccines for better results |
You can look forward to safer, more effective cancer care and new hope for the future.
FAQ
What is a cancer vaccine?
A cancer vaccine trains your immune system to find and attack cancer cells. You get a shot that helps your body recognize cancer as a threat. This helps stop cancer from growing or coming back.
Are cancer vaccines safe?
You usually experience mild side effects, such as soreness or tiredness. Most people do not have serious problems. Doctors watch you closely during treatment to keep you safe.
Who can get a cancer vaccine?
You may get a cancer vaccine if you have certain types of cancer or if you are at high risk. Your doctor checks your health and cancer type before recommending a vaccine.
How do mRNA cancer vaccines work?
mRNA cancer vaccines give your cells instructions to make proteins found in cancer. Your immune system learns to attack these proteins. This helps your body fight cancer more effectively.
Will cancer vaccines replace other treatments?
You still need other treatments, such as surgery or chemotherapy. Cancer vaccines often work best when combined with these therapies. Your doctor creates a plan that fits your needs.
See Also
Exploring Cancer Types Associated With AIDS Infection
An In-Depth Overview of Various Cancer Types
Recognizing Symptoms and Treatments for Duodenal Cancer
Key Features and Insights Into Cholangiocarcinoma
Insights Into Large Cell Lung Carcinoma With Rhabdoid Traits

