Tobacco Atlas Shows Shifting U.S. Health Gaps

The U.S. Tobacco Atlas reveals that cigarette smoking rates have dropped across the country. The latest data show these numbers:
Category | Percentage |
|---|---|
Overall Adult Smoking | |
Men | 22.9% |
Women | 15.8% |
Youth (ages 10-14) | 3.6% |
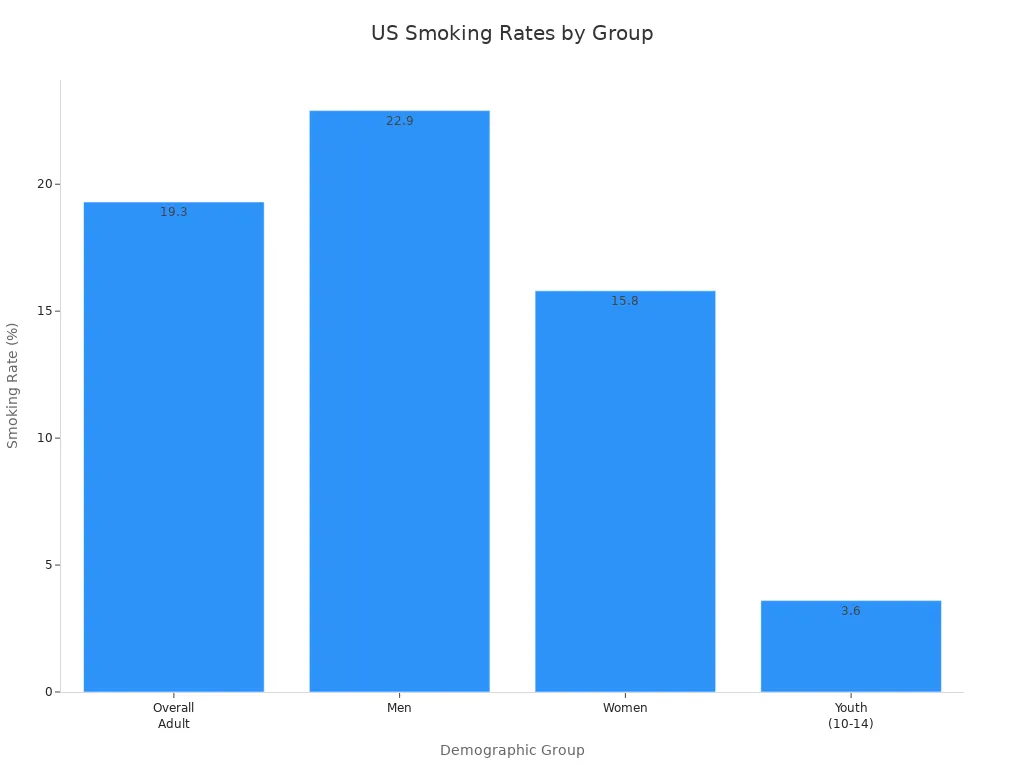
Marginalized groups face higher tobacco use and lower success when quitting. These gaps create serious health problems and show that current policies do not reach everyone. The Atlas gives public health leaders and policymakers the facts they need and urges stronger, fairer tobacco control efforts to protect all communities.
Key Takeaways
Cigarette smoking rates in the U.S. have significantly decreased, with adult smoking dropping from 21.2% in 2011 to 12.1% in 2023.
Marginalized groups experience higher tobacco use and face greater challenges in quitting, highlighting the need for targeted public health policies.
E-cigarette use is rising, especially among youth, with 1.63 million young people using e-cigarettes in 2023, raising new concerns for tobacco control.
Secondhand smoke exposure has decreased, but it still poses serious health risks, particularly for low-income and less educated individuals.
Stronger tobacco control policies, including smoke-free laws and higher taxes, are essential to reduce tobacco-related harm and health disparities.
U.S. Tobacco Atlas Overview

Purpose and Structure
The U.S. Tobacco Atlas launched as a new resource for public health. The creators designed it to raise awareness and influence policy about tobacco’s impact on health, politics, and business. The Atlas uses both a print edition and a companion website. The website helps more people access information and see updated research and graphs. The American Cancer Society and Vital Strategies worked together to build the Atlas. They wanted to turn complex data into stories that people can understand. The Atlas uses illustrations to show the serious problems caused by tobacco. These images help readers see the real effects of tobacco use.
The Atlas presents information in a clear way. The print edition highlights key facts and figures. The website gives users more details and new research. The team behind the Atlas believes that sharing data in different formats helps more people learn and take action.
The U.S. Tobacco Atlas combines strong visuals and easy-to-read data to make tobacco issues clear for everyone.
Objective/Component | Description |
|---|---|
Purpose | To raise awareness and influence public policy regarding the effects of tobacco on health, politics, and corporate behavior. |
Design | A new companion website was created alongside the print edition to enhance accessibility and engagement. |
Collaboration | Developed in partnership with the American Cancer Society and Vital Strategies to transform complex data into a compelling narrative. |
Visual Language | Illustrations were commissioned to effectively communicate serious issues related to tobacco. |
Data Presentation | The print edition highlights key data, while the website provides updated research and graphs. |
Key Audiences
The U.S. Tobacco Atlas speaks to many groups. Policymakers use the Atlas to guide decisions and create better laws. Public health leaders rely on the Atlas to plan programs and track progress. Teachers and students find the Atlas helpful for learning about tobacco’s impact. Community groups use the Atlas to support local efforts and raise awareness. The Atlas also reaches people who want to quit tobacco or help others stop. By sharing facts and stories, the Atlas encourages everyone to take action against tobacco use.
Tobacco Use Trends
Declining Smoking Rates
Cigarette smoking in the United States has dropped sharply over the past decade. The U.S. Tobacco Atlas shows that adult smoking rates fell by 43% from 2011 to 2023, moving from 21.2% to 12.1%. This decline happened in every state. The largest drops appeared in the District of Columbia and Rhode Island. Middle and high school students also smoked less. From 2011 to 2021, middle school smoking dropped by 50%, and high school smoking fell by 55%.
Trend Description | Percentage Change | Year Range |
|---|---|---|
Decrease in middle school smoking | 50% | 2011-2021 |
Decrease in high school smoking | 55% | 2011-2021 |
Public health policies helped drive these changes. Excise taxes and smoke-free air laws made a big difference. For example, between 2011 and 2013, the average adult smoking rate dropped from 21.3% to 19.3%. These laws made it harder to smoke in public and raised the cost of cigarettes.
Smoking rates differ by age and group. Adults aged 45–64 have the highest cigarette smoking rates. Non-Hispanic American Indian or Alaska Native adults, people with disabilities, and those with severe mental health issues smoke more than other groups. The U.S. Tobacco Atlas points out that men smoke more than women, but both groups have seen declines.
Year | Female Smoking Rate | |
|---|---|---|
2017 or earlier | 15.8% | 12.2% |
2020 | 10.07% | 8.44% |
2024 | 17.1% | 14.1% |
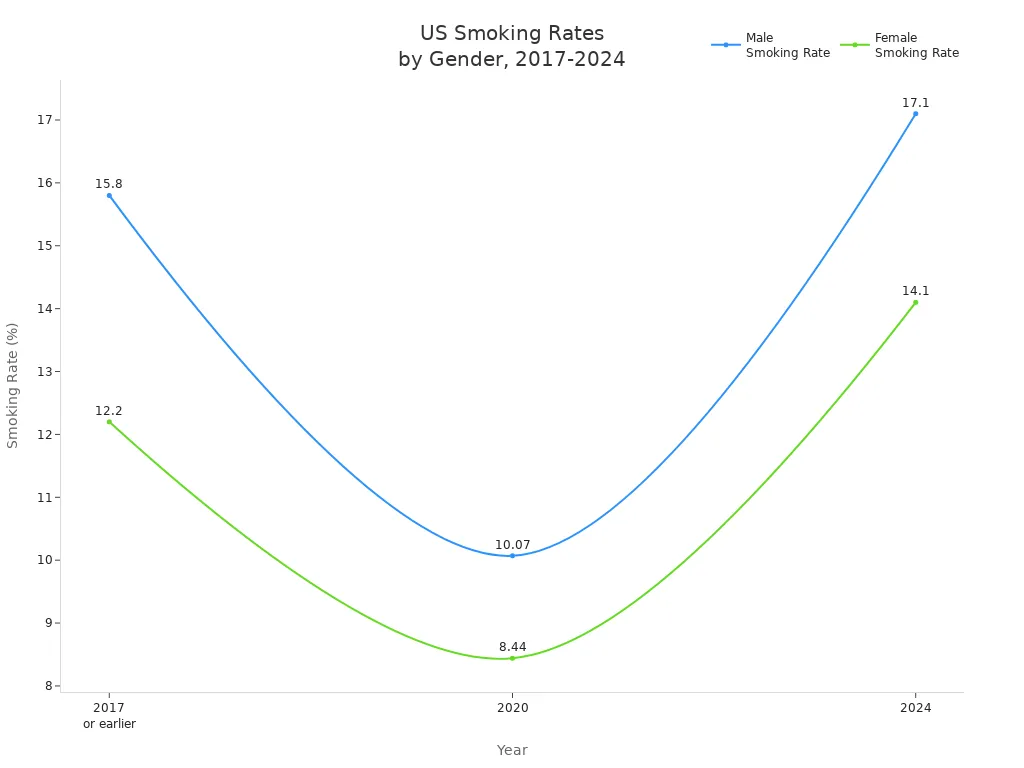
Smoking rates have dropped, but millions of Americans still smoke. Many belong to groups that face more health risks and less support.
E-Cigarette and Alternative Product Use
While cigarette smoking has gone down, e-cigarette use has gone up, especially among young people. In 2022, about 825,000 more children used e-cigarettes. Young adults aged 18–24 use e-cigarettes the most. In 2023, 15.5% of young adults (ages 21–24) used e-cigarettes, compared to 6.5% of all adults.
Year | Percentage of Adult E-Cigarette Users |
|---|---|
2019 | 4.5% |
2023 | 6.5% |
Young adults (ages 21-24) | 15.5% (2023) |
Men vs Women | Men more likely than women |
Youth e-cigarette use is a growing concern. In 2023, 1.63 million youth used e-cigarettes. High school students had a use rate of 7.8%, while middle school students had a rate of 3.5%. Many students use flavored products, and over one-third use e-cigarettes on most days.
Statistic | Value |
|---|---|
Total youth e-cigarette users | 1.63 million (5.9%) |
Middle school users | 410,000 (3.5%) |
High school users | 1.21 million (7.8%) |
Flavored e-cigarette users | 87.6% |
Daily users | 26.3% |
Students wanting to quit | 63.9% |
Students trying to quit | 67.4% |
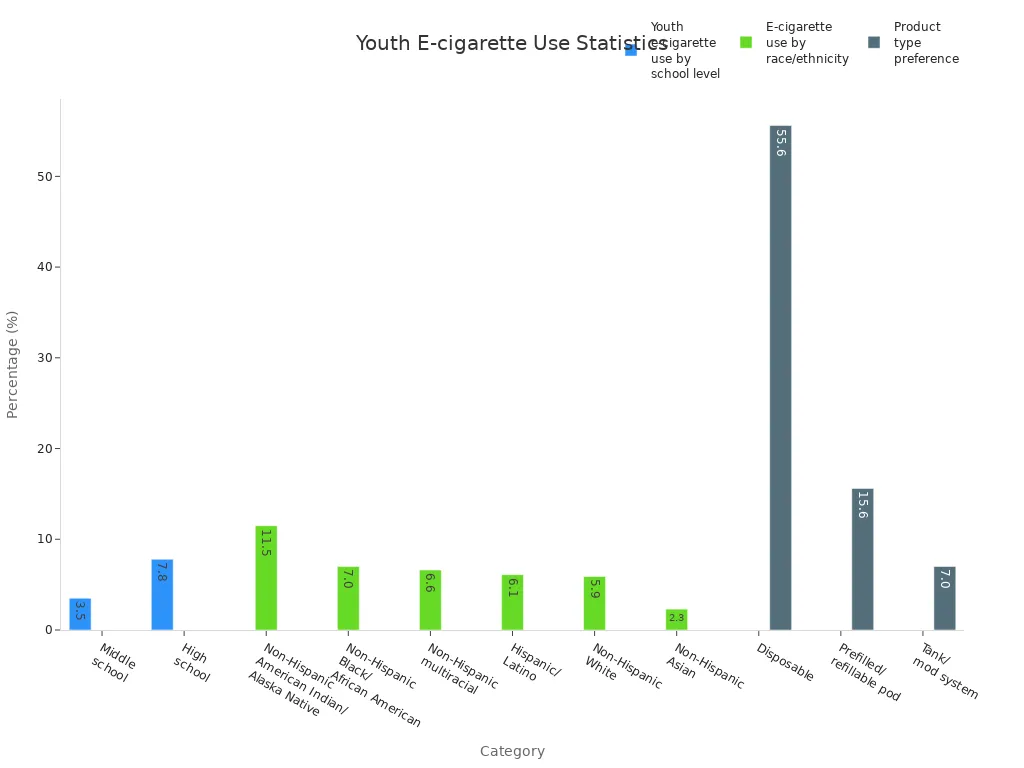
E-cigarette use also varies by race and ethnicity. Non-Hispanic American Indian or Alaska Native youth have the highest rates at 11.5%. Many students use more than one tobacco product. High school students report a 36.6% rate of using multiple products.
The rise in e-cigarette use among youth and young adults presents a new challenge for tobacco control efforts.
Secondhand Smoke Exposure
Secondhand smoke remains a serious health risk. Over the last decade, fewer nonsmoking adults have been exposed to secondhand smoke. The percentage dropped from 27.7% in 2009–2010 to 20.7% in 2017–2018.
Year Range | Prevalence of Secondhand Smoke Exposure (%) |
|---|---|
2009-2010 | 27.7 |
2017-2018 | 20.7 |
Secondhand smoke contains over 7,000 chemicals, including about 70 known to cause cancer.
Breathing in secondhand smoke can lead to lung cancer, heart disease, and stroke.
Each year, more than 19,000 deaths in the U.S. are linked to secondhand smoke.
Children exposed to secondhand smoke face higher risks for asthma attacks, respiratory infections, and sudden infant death syndrome (SIDS).
Disparities in exposure still exist. People with lower income or less education are more likely to be exposed. The U.S. Tobacco Atlas highlights that, even with progress, secondhand smoke continues to harm many Americans.
Reducing secondhand smoke exposure saves lives and improves health for everyone.
Health Impacts and Screening
Cancer and Tobacco
Tobacco use causes more cancer deaths than any other preventable factor in the United States. Over 80% of lung cancer deaths link directly to smoking. In 2023, smoking rates dropped to 11%, but tobacco still accounts for about 30% of all cancer deaths each year. The U.S. Tobacco Atlas reports that tobacco leads to 480,000 deaths annually. Doctors diagnose 660,000 new tobacco-related cancer cases every year, and 343,000 people die from these cancers.
Evidence Type | Data |
|---|---|
Annual Deaths Due to Tobacco | 480,000 |
Annual Tobacco-Related Cancer Diagnoses | 660,000 |
Annual Tobacco-Related Cancer Deaths | 343,000 |
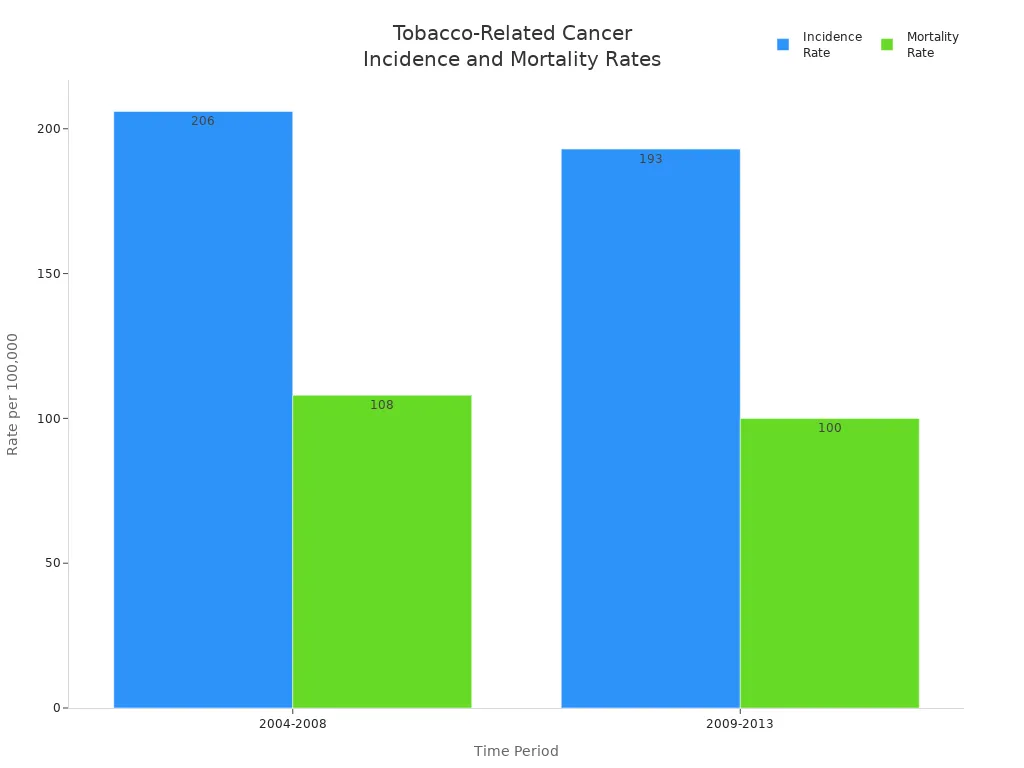
Incidence Rate of Tobacco-Related Cancer (2004-2008) | 206 per 100,000 |
Incidence Rate of Tobacco-Related Cancer (2009-2013) | 193 per 100,000 |
Mortality Rate of Tobacco-Related Cancer (2004-2008) | 108 per 100,000 |
Mortality Rate of Tobacco-Related Cancer (2009-2013) | 100 per 100,000 |
Lung Cancer Deaths Attributable to Smoking | 80% |
Lung Cancer Screening Gaps
Lung cancer screening saves lives, but many people miss out. In 2021, only 5.8% of eligible Americans received a lung cancer screening. Massachusetts had the highest rate at 16.3%. California and Nevada had rates below 2%. More than 40% of lung cancer cases are found late, and survival drops below 9%. Annual low-dose CT scans can lower lung cancer deaths by 20% for high-risk groups.
Current guidelines may not include many racial minorities, which leads to fewer screenings.
Simplified rules could help more Black and white people qualify for screening.
Over 14 million Americans qualify for screening, but many do not know about it.
In one study, only 43% of Black women with lung cancer qualified for screening.
Most people who qualify do not get screened, often because they lack awareness or access.
Evidence Type | Findings |
|---|---|
Lung Cancer Screening | LDCT reduces lung cancer mortality by 20% compared to CXR screening |
Smoking Cessation | Abnormal screening results lead to a 6% lower smoking rate in individuals with abnormal results compared to normal results |
Teachable Moment | Screening results can encourage smoking cessation interventions, enhancing overall health outcomes |
Smoking Cessation Challenges
Quitting smoking remains difficult for many Americans. Several barriers stand in the way:
Cultural norms in addiction treatment centers support smoking.
Many clients feel unready to quit.
Clinics often lack resources for nicotine replacement therapy and staff training.
Staff members who smoke may influence clients.
Tobacco outlets near treatment centers make quitting harder.
"One of the barriers is that behavioral health clinicians are not really… schooled and trained to address nicotine addiction in that context. So it’s not part of the culture."
Successful interventions include advice from healthcare providers, workplace programs, media campaigns, and technology-based tools.
Intervention Type | Evidence of Effectiveness |
|---|---|
Healthcare Provider Involvement | Brief advice from physicians can increase quit rates, especially with follow-up. |
Employer-Based Programs | Successful programs link to workplace smoking bans and offer incentives like free nicotine replacement therapy. |
Media Campaigns | Effective in motivating smokers to quit and changing social norms; emotional ads are more effective than humorous ones. |
Technology-Based Interventions | High potential reach; some studies show positive results, but evidence is inconsistent due to methodological challenges. |
Disparities and Policy Gaps
Marginalized Populations
Many marginalized groups in the United States face higher risks from tobacco. Systemic inequities make it harder for these communities to avoid tobacco use and get help to quit. The tobacco industry often targets low-income and diverse neighborhoods with advertising and promotions. Limited access to healthcare resources means fewer opportunities for prevention and treatment. Social factors like education and discrimination also increase tobacco use risk.
People with low socioeconomic status struggle to get healthcare and manage smoking-related health problems.
Uninsured individuals miss out on screenings and care, which leads to worse health outcomes.
Delays in healthcare due to low income cause more health complications.
Web-based quitlines and FDA-approved cessation medications are less accessible to racial and ethnic minorities.
Regional Differences
Tobacco use and health impacts vary across regions and communities. Black Americans have similar smoking rates to white Americans, but menthol cigarette use is much higher among Black Americans (88.5% vs. 29%). Death rates from tobacco-related diseases are also higher in Black communities. The tobacco industry has a history of targeting Black, Brown, and Indigenous peoples with menthol marketing and cultural exploitation.
Community Type | Smoking Rate | Menthol Cigarette Use | Death Rate |
|---|---|---|---|
Black Americans | Similar | 88.5% | Higher than white Americans |
White Americans | Similar | 29% | Lower than Black Americans |
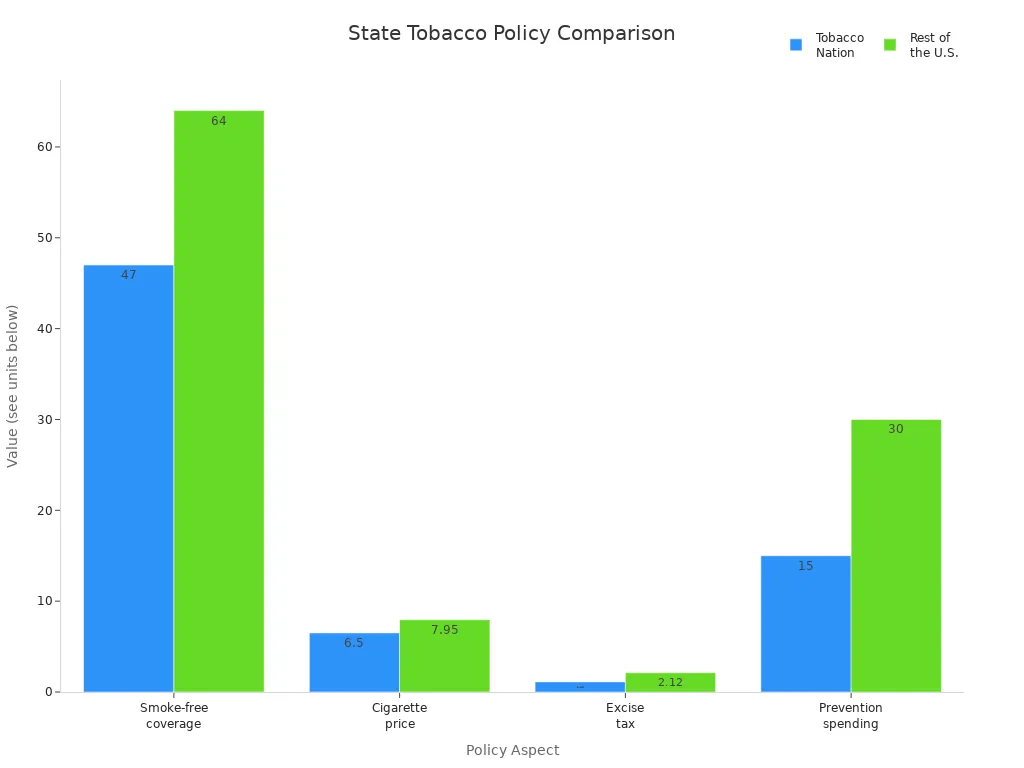
State-level policies show big gaps. Tobacco Nation states have higher smoking rates and weaker tobacco control laws. These states spend less on prevention and have lower cigarette prices and excise taxes.
Aspect | Tobacco Nation | Rest of the U.S. |
|---|---|---|
Coverage by smoke-free policies | 47% | 64% |
Average cigarette price | $6.50 | $7.95 |
Average excise tax | $1.11 | $2.12 |
Spending on prevention programs | <15% | 30% |
Policy Needs and Solutions
Stronger and fairer tobacco control policies can help close these gaps. Many governments have not adopted all recommended measures, such as comprehensive smoke-free laws and higher taxes. Regulations on nicotine and flavored tobacco products remain weak in many areas. Experts recommend several solutions:
Implement smoke-free policies in all public indoor spaces and workplaces.
Limit nicotine levels in tobacco products.
Ban flavored tobacco, including menthol, to protect youth and vulnerable groups.
Control the number and location of tobacco stores in high-risk areas.
Raise tobacco prices and remove discounts.
Expand support for quitlines and cessation resources.
Launch educational campaigns for all communities.
Equitable policies and strong enforcement can reduce tobacco-related harm and save lives.
The U.S. Tobacco Atlas shows that strong leadership and new policies remain urgent to reduce tobacco-related harm and health disparities. Experts recommend actions such as removing flavored tobacco, increasing federal investment, improving access to treatment, and promoting research.
Recommendation | Description |
|---|---|
Strengthen policies | Restrict manufacture, sale, and marketing of tobacco products. |
Increase federal investment | Enhance funding for tobacco control programs. |
Improve access to treatment | Ensure low-cost, high-quality options for tobacco dependence. |
Promote research | Support studies on health effects and new treatments. |
Advocates, health experts, and governments must work together. The Atlas highlights the need for collaboration and comprehensive tobacco control. Communities can pool resources, create tailored plans, and drive change. Collective action offers hope to end the tobacco epidemic.
FAQ
What is the U.S. Tobacco Atlas?
The U.S. Tobacco Atlas is a resource that shows data about tobacco use, health impacts, and policies. The American Cancer Society and Vital Strategies created it to help people understand tobacco issues.
Who uses the U.S. Tobacco Atlas?
Policymakers, health leaders, teachers, and community groups use the Atlas. They rely on it to guide decisions, plan programs, and teach others about tobacco risks.
Why do some groups have higher tobacco use?
Many marginalized groups face more tobacco advertising and have less access to healthcare. Social and economic factors make quitting harder for these communities.
The Atlas highlights these disparities and urges action to support all groups.
How can people quit smoking?
People can quit smoking with help from doctors, quitlines, and support programs. Nicotine replacement therapy and counseling increase success rates. Technology-based tools also help many people stop using tobacco.
See Also
Recognizing Symptoms And Causes Of Esophageal Cancer
Exploring Cancer Types Associated With AIDS Infection
An In-Depth Overview Of Various Cancer Types

