What Is Uterine Sarcoma and Its Main Types

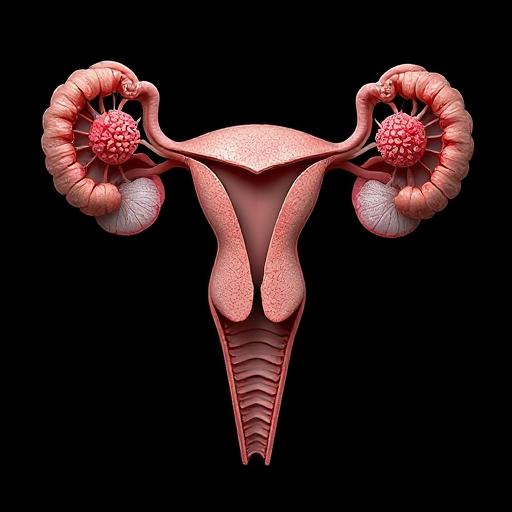
Uterine sarcoma is a rare type of cancer that develops in the muscles or connective tissues of the uterus. It accounts for only 2% to 5% of all uterine cancers, making it an uncommon but serious condition. Unlike endometrial cancer, which starts in the uterine lining, uterine sarcoma originates in the muscle layer and connective tissues. This biological difference sets it apart from other uterine cancers. The disease is more common in individuals over 40, with an average diagnosis age of 60. Black women also face a higher risk, with incidence rates twice as high as those in white women.
Key Takeaways
Uterine sarcoma is a rare cancer in the uterus. It grows in the muscles or connective tissues. Finding it early helps with better treatment.
There are different types of uterine sarcoma. These include leiomyosarcoma, endometrial stromal sarcoma, and undifferentiated sarcoma. Each type is treated differently.
Common signs of uterine sarcoma are unusual bleeding, pelvic pain, or a lump. See a doctor quickly if you notice these symptoms.
Things that raise the risk include age, pelvic radiation, or certain genetic issues. Knowing these risks can help find it early.
Surgery is the main way to treat uterine sarcoma. Chemotherapy or hormone therapy may follow. Talk to your doctor about the best treatment for you.
Types of Uterine Sarcoma

Leiomyosarcoma
Leiomyosarcoma is the most common type of uterine sarcoma. It develops in the smooth muscle walls of the uterus, known as the myometrium. This type accounts for about 30% of all uterine sarcomas. You may find it helpful to know that uterine sarcomas, in general, make up only 2% to 5% of all uterine cancers. Leiomyosarcoma tends to grow quickly and can spread to other parts of the body.
Unlike other types, leiomyosarcoma often presents with symptoms like abnormal bleeding, pelvic pain, or a noticeable mass in the abdomen. Early detection plays a crucial role in managing this aggressive cancer.
Endometrial Stromal Sarcoma
Endometrial stromal sarcoma forms in the connective tissue that supports the uterine lining. It is less common than leiomyosarcoma, making up about 15% of uterine sarcomas. This type is further divided into low-grade and high-grade forms. Low-grade tumors grow slowly, while high-grade ones are more aggressive.
Type of Tumor | Percentage |
|---|---|
Uterine Leiomyosarcoma (u-LMS) | 63% |
High-Grade Endometrial Stromal Sarcoma | 21% |
Low-Grade Endometrial Stromal Sarcoma | 21% |
Undifferentiated Uterine Sarcoma | 5% |
Endometrial stromal sarcoma differs from other uterine sarcomas due to its slower progression in low-grade cases. You may notice symptoms like heavy menstrual bleeding or pelvic discomfort.
Undifferentiated Sarcoma
Undifferentiated sarcoma is the rarest type of uterine sarcoma, accounting for only 5% of cases. It is highly aggressive and difficult to treat. This type lacks the distinct features seen in other sarcomas, making diagnosis challenging.
Survival rates for undifferentiated sarcoma vary based on the stage at diagnosis. For localized cases, the 5-year survival rate is 71%. However, this drops significantly for distant-stage cases, with a survival rate of only 18%. You should consult a healthcare provider immediately if you experience persistent symptoms like unexplained bleeding or pelvic pain.
Adenosarcoma
Adenosarcoma is a rare type of uterine sarcoma that combines both glandular (adeno) and mesenchymal (sarcoma) tissue components. It typically develops in the endometrium, the inner lining of the uterus, but it can also arise in other parts of the reproductive system. This type of cancer is considered a low-grade tumor, meaning it grows slowly compared to other uterine sarcomas. However, it can still invade surrounding tissues if left untreated.
You may notice symptoms such as abnormal vaginal bleeding, pelvic pain, or a noticeable mass in the lower abdomen. These signs often overlap with other uterine conditions, making early diagnosis essential. Doctors usually confirm adenosarcoma through a biopsy and imaging tests like ultrasounds or MRIs.
Treatment for adenosarcoma often involves surgery to remove the uterus (hysterectomy). In some cases, additional therapies like radiation or chemotherapy may be necessary, especially if the cancer has spread. Regular follow-ups are crucial to monitor for recurrence.
Uterine Carcinosarcoma
Uterine carcinosarcoma, also known as malignant mixed Müllerian tumor (MMMT), is an aggressive form of uterine sarcoma. It contains both carcinoma (epithelial cancer) and sarcoma (connective tissue cancer) components. This dual nature makes it particularly challenging to treat. Carcinosarcoma accounts for about 5% of all uterine cancers but represents a significant portion of uterine sarcoma cases.
You might experience symptoms like heavy vaginal bleeding, pelvic pain, or an enlarged uterus. These symptoms often mimic those of other uterine conditions, which can delay diagnosis. Doctors typically use imaging tests and biopsies to identify carcinosarcoma.
Treatment usually begins with surgery to remove the uterus, ovaries, and fallopian tubes. Chemotherapy often follows to target any remaining cancer cells. Radiation therapy may also be recommended in some cases. Early detection and a comprehensive treatment plan improve the chances of managing this aggressive cancer effectively.
Symptoms of Uterine Sarcoma
Common Symptoms
Recognizing the symptoms of uterine sarcoma early can make a significant difference in treatment outcomes. You may notice several warning signs that should prompt a visit to your healthcare provider. These include:
Abnormal vaginal bleeding, such as bleeding between periods, heavier-than-usual periods, or bleeding after menopause.
Vaginal discharge that may occur without blood and does not improve with medication.
Pelvic or abdominal pain, which can range from mild discomfort to severe cramping.
A palpable mass in the pelvis or vagina, which you might feel as a lump or swelling.
Frequent urination or difficulty emptying your bladder completely.
Constipation or a feeling of fullness in the abdomen.
These symptoms often appear suddenly and may worsen over time. If you experience any of these signs, consult a healthcare professional promptly. Early detection is crucial for managing uterine sarcoma effectively.
Symptoms Overlapping with Other Uterine Conditions
Some symptoms of uterine sarcoma overlap with those of benign conditions like fibroids, making diagnosis challenging. For example, abnormal vaginal bleeding and pelvic pain are common in both uterine sarcoma and fibroids. However, certain signs, such as bleeding after menopause or vaginal discharge that doesn’t improve with antibiotics, are more specific to uterine sarcoma.
Symptom | Uterine Sarcoma | Benign Conditions (e.g., Fibroids) |
|---|---|---|
Abnormal vaginal bleeding | Yes | Yes |
Pelvic pain | Yes | Yes |
Bleeding after menopause | Yes | No |
Vaginal discharge | Yes (not improving with antibiotics) | No |
Presence of a mass | Yes | Yes |
If you experience unusual bleeding, discharge, or other persistent symptoms, report them to your doctor. While benign conditions are more common, it’s essential to rule out serious issues like uterine sarcoma. Diagnostic tests, including imaging and biopsies, can help differentiate between these conditions.
Risk Factors for Uterine Sarcoma
Known Risk Factors
Certain factors increase your likelihood of developing uterine sarcoma. These include:
Pelvic radiation therapy: If you’ve undergone radiation treatment for cancers like cervical or rectal cancer, your risk rises. This increased risk often appears 5 to 25 years after treatment.
Congenital retinoblastoma: This rare, inherited eye cancer raises the chance of developing soft tissue sarcomas, including uterine sarcoma.
Family history of kidney cancer: A genetic condition called hereditary leiomyomatosis and renal cell cancer (HLRCC) links kidney cancer to uterine sarcoma.
Tamoxifen use: Women taking tamoxifen for breast cancer face a slightly higher risk. This risk typically emerges 2 to 5 years after starting the medication.
Evidence Type | Description |
|---|---|
Risk Factor | Pelvic radiation therapy increases the risk of uterine sarcoma. |
Timeframe | Increased risk typically manifests 5 to 25 years after radiation treatment. |
If any of these factors apply to you, consider discussing them with your doctor. Early awareness can help you take proactive steps.
Other Contributing Factors
Age plays a significant role in the development of uterine sarcoma. Women aged 50 and older face a much higher risk compared to younger women. For every 10 women in this age group, approximately 6.4 are diagnosed, compared to only 1.5 in younger women. Older women also experience worse survival rates, with a hazard ratio of 1.78 indicating a higher risk of mortality.
Genetic mutations also contribute to uterine sarcoma. Specific mutations, such as TP53, RB1, and ATRX, are linked to uterine leiomyosarcoma. Fusion proteins like JAZF1–SUZ12 and chromosomal translocations like t(7;17)(p15;q21) are associated with endometrial stromal sarcomas.
Gene/Mutation | Type of Mutation | Associated Sarcoma Type |
|---|---|---|
TP53 | Mutation | Uterine Leiomyosarcoma |
RB1 | Mutation | Uterine Leiomyosarcoma |
ATRX | Mutation | Uterine Leiomyosarcoma |
JAZF1–SUZ12 | Fusion Protein | Low-Grade Endometrial Stromal Sarcoma |
t(7;17)(p15;q21) | Chromosomal Translocation | Low-Grade Endometrial Stromal Sarcoma |
Understanding these contributing factors can help you assess your risk and seek medical advice if needed.
Treatment Options for Uterine Sarcoma
Surgery
Surgery is the primary treatment for uterine sarcoma. It aims to remove the cancerous tissue and prevent its spread. The type of surgery depends on the tumor's stage and location. Common procedures include:
Laparotomy: A large incision in the abdomen to examine the uterus and surrounding tissues.
Total Abdominal Hysterectomy: Removal of the uterus and cervix through an abdominal incision.
Bilateral Salpingo-Oophorectomy: Removal of both ovaries and fallopian tubes.
Lymphadenectomy: Removal of lymph nodes to check for cancer spread.
Surgical Procedure | Description |
|---|---|
Total Hysterectomy | Removal of the entire uterus with the cervix. |
Radical Hysterectomy | More extensive surgery, including removal of surrounding tissues. |
Bilateral Salpingo-Oophorectomy | Removal of both ovaries and fallopian tubes. |
Lymph Node Surgery | Removal of lymph nodes to check for cancer spread. |
Hysterectomy is often performed when malignancy is suspected. The extent of surgery depends on the tumor's progression. Early-stage surgeries have higher success rates, making timely diagnosis essential.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth. It is often recommended when uterine sarcoma has spread or cannot be fully removed surgically. A combination of gemcitabine and docetaxel has shown a 53% response rate in patients with unresectable leiomyosarcomas. This regimen is now a global standard for advanced cases.
Common chemotherapy drugs include:
Doxorubicin
Docetaxel
Gemcitabine
Ifosfamide
Trabectedin
While effective, chemotherapy can cause side effects such as nausea, fatigue, and hair loss. Some drugs, like doxorubicin, may lead to long-term complications, including heart damage. Discuss potential risks and benefits with your doctor to make informed decisions.
Hormonal Therapy
Hormonal therapy targets cancer cells that rely on hormones like estrogen and progesterone for growth. This treatment blocks the hormones or prevents cancer cells from accessing them, leading to their shrinkage or death. Endometrial stromal sarcoma responds particularly well to hormonal therapy.
Hormonal therapy is often used:
After surgery to reduce recurrence risk.
When cancer has spread or recurred.
If surgery or radiation is not viable.
Drugs that block hormone activity may be prescribed based on the sarcoma type. This approach offers a less invasive option for managing certain uterine sarcomas effectively.
Uterine sarcoma is a rare but aggressive cancer that demands early detection for better outcomes. Early diagnosis enables precise surgical planning and helps evaluate the spread of the disease. For example, preoperative sampling plays a vital role in identifying distant metastasis. Survival rates vary significantly based on the stage at diagnosis. Low-grade endometrial stromal sarcoma has a 5-year survival rate of over 99.5% when localized, while advanced stages of leiomyosarcoma show only a 12% survival rate. Adopting healthy habits like eating well and staying active can also improve outcomes. Always consult your doctor for personalized care.
FAQ
What makes uterine sarcoma different from other uterine cancers?
Uterine sarcoma develops in the muscles or connective tissues of the uterus, while other uterine cancers, like endometrial cancer, form in the uterine lining. This difference affects symptoms, diagnosis, and treatment approaches.
Can uterine sarcoma be detected early?
Early detection is challenging because symptoms often overlap with benign conditions. However, paying attention to unusual signs like postmenopausal bleeding or persistent pelvic pain can help you seek timely medical advice.
Is uterine sarcoma hereditary?
Most cases are not hereditary. However, genetic conditions like hereditary leiomyomatosis and renal cell cancer (HLRCC) can increase your risk. Discuss your family history with a doctor to assess your risk.
How can you reduce the risk of uterine sarcoma?
While you cannot eliminate the risk, maintaining a healthy lifestyle and avoiding unnecessary exposure to radiation or hormone therapies like tamoxifen may help lower your chances.
What should you do if you suspect uterine sarcoma?
Consult a healthcare provider immediately. They may recommend imaging tests, biopsies, or other diagnostic procedures to confirm the condition and plan treatment.
Tip: Keep track of any unusual symptoms and share them with your doctor for a more accurate diagnosis.
See Also
Exploring Gestational Trophoblastic Tumors And Their Varieties
Identifying Leiomyosarcoma: Symptoms You Should Be Aware Of
Fibrosarcoma Explained: Key Features And Insights To Know
Malignant Fibrous Histiocytoma And Osteosarcoma: A Comprehensive Overview

