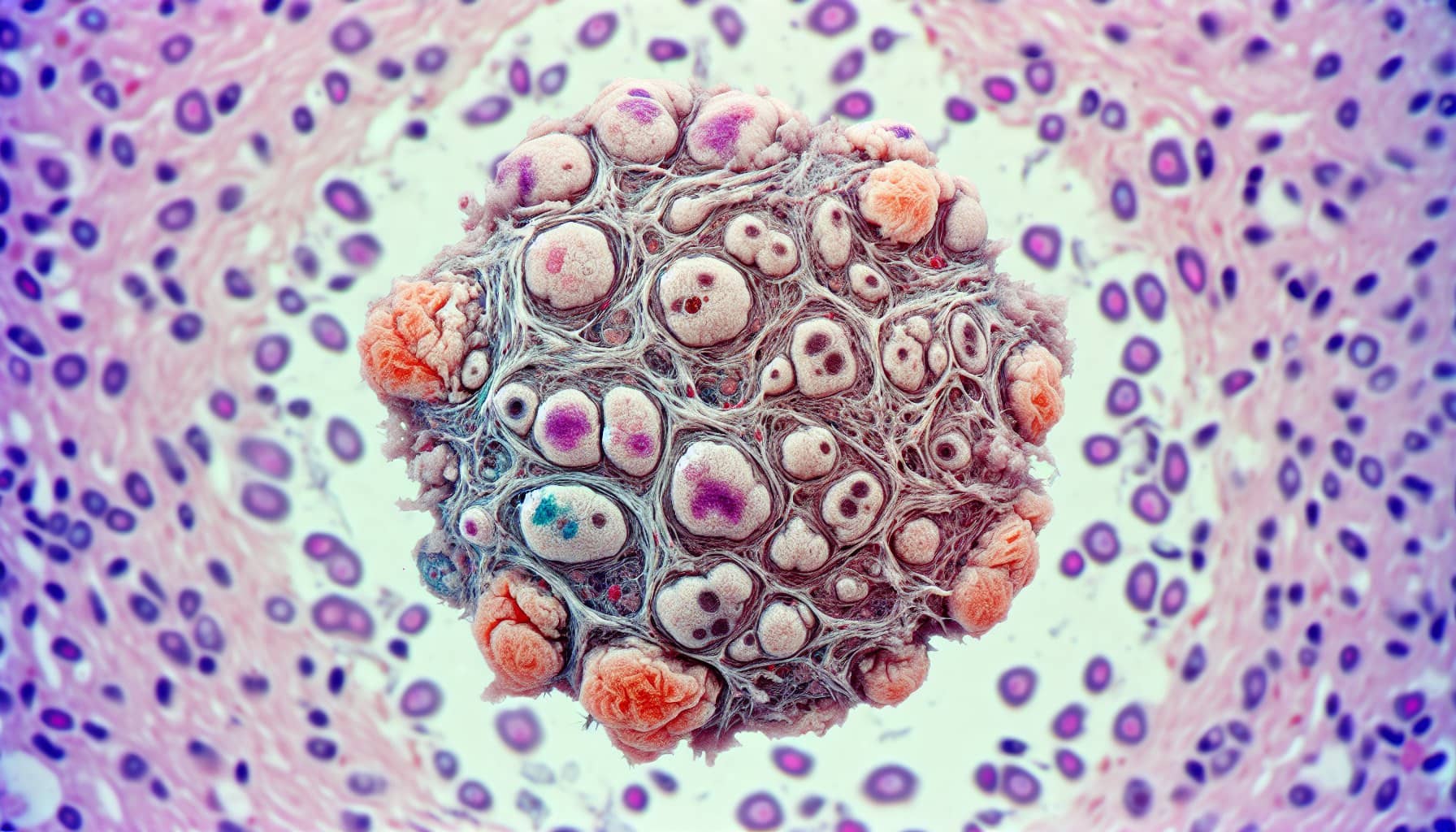
What is Ependymoma and Its Symptoms Explained
Ependymoma is a rare tumor that develops in the brain or spinal cord. It can affect both children and adults, though it accounts for only 2% of brain and spinal cord tumors in adults and 5% in children. The symptoms you may experience depend on the tumor's location, your age, and the tumor's growth rate. Common signs include headaches, nausea, dizziness, and weakness. In children, symptoms like irritability or developmental delays may appear. If the tumor forms in the spinal cord, you might notice back pain, numbness, or changes in bowel habits.
Key Takeaways
Ependymoma is a rare tumor in the brain or spine. It can affect both kids and adults. Spotting symptoms like headaches or back pain early is important for better results.
Symptoms depend on where the tumor is. Brain tumors might cause headaches or confusion. Spinal tumors can cause back pain or weakness. Knowing these signs helps you get medical care quickly.
Treatment usually starts with surgery to remove the tumor. If the whole tumor can't be removed, radiation therapy might be needed. Learning about treatments helps patients make good choices.
Support is very important for getting better. Staying healthy, being active, and finding emotional help can make life better after treatment.
Regular check-ups and imaging tests are key to tracking progress. They also help find out if the tumor comes back. Taking care of your health can lead to better results over time.
Symptoms of Ependymoma
Symptoms Based on Location
Brain Tumors
The symptoms of brain ependymomas vary depending on the tumor's location. Tumors in the supratentorial region often cause headaches, nausea, vomiting, seizures, and behavioral changes. You might also experience confusion, vision problems, or weakness. Tumors in the posterior fossa can lead to lethargy, unsteady gait, and nausea. Babies with posterior fossa tumors may show a rapidly growing head circumference. The table below summarizes these symptoms:
Tumor Location | Common Symptoms |
|---|---|
Supratentorial | Headache, nausea, vomiting, seizures, behavioral changes, confusion, vision problems, weakness |
Posterior Fossa | Headache, nausea, vomiting, lethargy, unsteady gait, rapidly growing head circumference in babies |
Spinal Cord Tumors
Spinal cord ependymomas often present with back or neck pain. You may notice weakness, numbness, or tingling in your arms or legs. Changes in bowel patterns, incontinence, and difficulty with coordination or balance are also common. Symptoms can vary based on the tumor's location in the spinal cord:
Cervical levels: Weakness or motor dysfunction in the upper limbs.
Thoracic levels: Sensory symptoms, such as loss of sensation below the lesion.
Lumbar levels: Radicular pain and weakness in the lower limbs.
Symptoms Based on Age
Children
In children, ependymomas can cause irritability, developmental delays, and difficulty walking. Younger children may also experience vomiting, lethargy, or an increase in head size due to fluid buildup in the brain.
Adults
Adults with ependymomas often report headaches, nausea, and dizziness. You might also experience back pain, weakness, or sensory changes, depending on the tumor's location.
Symptoms Based on Tumor Type
Slow-Growing Tumors
Slow-growing ependymomas may not cause symptoms for years. These tumors are often discovered incidentally during imaging for unrelated issues.
Rapidly Growing Tumors
Rapidly growing ependymomas, such as anaplastic ependymomas, tend to cause symptoms quickly. You may experience headaches, nausea, vomiting, and behavioral changes.
Causes and Types of Ependymoma
Causes of Ependymoma
The exact cause of ependymoma remains unclear, but researchers have identified several factors that may contribute to its development:
Genetic mutations, such as YAP1 and ZFTA fusions, are linked to ependymomas in specific brain regions.
Chromosomal abnormalities, particularly in chromosome 22, may play a role in tumor formation.
Neurofibromatosis type II (NF2), a rare genetic disorder, increases the risk of spinal ependymomas.
Developmental issues during early growth may lead to tumor formation later in life.
Most ependymomas occur sporadically, meaning they do not have a hereditary link. However, individuals with genetic conditions like NF2 face a higher likelihood of developing these tumors.
Types of Ependymoma
Subependymoma
Subependymoma is a slow-growing tumor classified as Grade I. It typically forms near the brain's ventricles or the spinal cord. This type accounts for about 8% of all ependymomas and is more common in males over 40 years old. Many patients do not experience symptoms, but when symptoms occur, they may include headaches, hydrocephalus, or neurological deficits depending on the tumor's location.
Myxopapillary Ependymoma
Myxopapillary ependymoma is another Grade I tumor, usually found in the spinal column. It grows slowly and has a favorable prognosis, especially when completely removed through surgery. This type is more common in adults and is often benign.
Anaplastic Ependymoma
Anaplastic ependymoma is a Grade III tumor, making it the most aggressive type. Its rapid cell growth and abnormal structure contribute to its malignancy. This type often leads to a poor prognosis due to its fast progression and resistance to treatment.
Diagnosis of Ependymoma
Medical History and Physical Examination
Diagnosing ependymoma begins with a detailed medical history and physical examination. Your doctor will ask about your symptoms, their duration, and any family history of cancer or brain tumors. This information is especially important for children, as parents often provide critical details about developmental delays or unusual behaviors.
During the physical examination, your doctor will perform several tests to assess your nervous system. These tests evaluate your coordination, reflexes, and strength. The table below outlines some common techniques used:
Examination Technique | Description |
|---|---|
Neurological Tests | Assess brain function through cognitive tests and look for signs of hydrocephalus. |
Nervous System Exam | Involves tasks like walking, touching your finger to your nose, and following a light with your eyes. |
Comprehensive Exam | Includes assessment of hearing, eye movements, sense of smell, sensation, motor function, swallowing, balance, and coordination. |
Initial Assessment | Review of symptoms, medical history, and a neurological examination to check vision, coordination, reflexes, and strength. |
Imaging Tests
MRI
Magnetic resonance imaging (MRI) is the most effective tool for identifying ependymoma. It provides high-resolution images that help pinpoint the tumor's location and characteristics. For example:
Supratentorial ependymomas often appear with variable signal intensity on T1- and T2-weighted images.
Posterior fossa tumors may invade through the foramen of Magendie, which MRI can detect.
Spinal ependymomas typically show hyperintensity on T2-weighted images, making MRI highly sensitive for these cases.
CT Scan
Although MRI is the gold standard, CT scans are sometimes used as an initial imaging study. They are particularly helpful when MRI is not an option, such as when a patient cannot tolerate the procedure. CT scans can quickly identify central nervous system lesions, providing a practical alternative in certain situations.
Biopsy and Pathology
If imaging tests suggest ependymoma, your doctor may recommend a biopsy. This procedure involves removing a small sample of tumor tissue for analysis. A neuropathologist examines the sample to determine the tumor's type and grade. Tumors are graded based on how the cells look under a microscope:
Grade I: Cells appear typical.
Grade II: Cells show slight abnormalities.
Grade III: Cells are highly atypical and grow rapidly.
This information is crucial for planning the most effective treatment for your condition.
Treatment Options for Ependymoma

Surgery
Surgery is often the first step in treating ependymoma. Your doctor may perform a craniotomy to access and remove the tumor. The goal is to achieve complete resection, but this depends on the tumor's location. If the tumor is near critical structures, only partial removal may be possible.
Several advanced surgical techniques improve precision and outcomes:
Microsurgery: A microscope helps the surgeon see fine details during the procedure.
Endoscopic neurosurgery: Small tubes with cameras allow minimally invasive access to the tumor.
Laminectomy or laminoplasty: These techniques are used for spinal tumors, involving the removal or repositioning of vertebral bones.
Surgical Technique | Description |
|---|---|
Craniotomy | Removes part of the skull to access and remove brain tumors. |
Laminectomy or Laminoplasty | Accesses spinal tumors by removing or repositioning vertebral bones. |
Minimally invasive method using a camera-equipped tube to remove tumors. |
While surgery is effective, complications can occur. These include hemorrhage, infection, or worsening neurological deficits. Children may experience cerebellar mutism, which affects speech temporarily. Long-term risks include spinal instability or sensory loss.
Radiation Therapy
Radiation therapy plays a key role, especially when complete tumor removal isn’t possible. It targets remaining cancer cells to prevent recurrence. For supratentorial ependymomas, conformal radiation is standard after incomplete resection. In posterior fossa tumors, radiation improves survival rates, particularly in the PF-A subtype. Spinal ependymomas may require radiation based on tumor grade and recurrence.
However, radiation therapy has side effects. You might experience fatigue, nausea, or hair loss. Skin changes like redness or swelling are common. Long-term effects include cognitive challenges or slowed growth in children. Despite these risks, radiation remains a critical tool in managing ependymoma.
Chemotherapy
Chemotherapy is not the primary treatment for ependymoma but can help in aggressive cases. It is often used for anaplastic ependymomas before or after radiation. This approach aims to destroy infiltrating tumor cells. In young children, chemotherapy may delay the need for radiation, reducing long-term side effects.
Common drugs include lapatinib and temozolomide, which show promise in treating ependymoma. While chemotherapy is less common, it provides an additional option when surgery and radiation are insufficient.
Supportive Care and Rehabilitation
Recovering from ependymoma involves more than just medical treatments. Supportive care and rehabilitation play a vital role in helping you regain strength, manage symptoms, and improve your quality of life. By taking an active role in your recovery, you can enhance your overall well-being.
Start by learning about your condition. Understanding ependymoma and its effects empowers you to make informed decisions about your care. Follow your doctor’s instructions carefully, including attending regular MRI scans and check-ups. These appointments help monitor your progress and detect any signs of recurrence early.
Maintaining a healthy lifestyle is equally important. Focus on eating a nutritious diet rich in fruits, vegetables, and lean proteins. Stay hydrated and aim for adequate sleep each night to support your body’s healing process. Regular exercise, tailored to your abilities, can improve your strength and energy levels. Physical therapists or rehabilitation specialists can guide you through exercises designed to restore mobility and reduce discomfort.
Emotional support is another key aspect of recovery. You may experience stress, anxiety, or even depression during this time. Speaking with a counselor or joining a support group can provide comfort and encouragement. Sharing your experiences with others who understand your journey can make a significant difference.
💡 Tip: Small steps, like staying active and seeking emotional support, can lead to big improvements in your recovery.
Rehabilitation doesn’t end with physical health. Emotional and mental well-being are just as important. By addressing all aspects of your recovery, you can build a strong foundation for a healthier future. Remember, every effort you make contributes to your journey toward healing and resilience.
Ependymoma is a rare tumor that can develop in the brain or spinal cord, causing symptoms like headaches, nausea, seizures, or back pain. Recognizing these signs early is critical for timely intervention, which can improve outcomes and, in some cases, lead to complete recovery. For aggressive forms like Grade 3 ependymomas, early detection helps manage symptoms and reduces the risk of recurrence.
You can take steps to identify potential symptoms, such as persistent headaches, memory problems, or weakness in your limbs. Regular follow-ups and imaging tests are essential for monitoring progress after treatment. Public awareness campaigns, like Ependymoma Awareness Day, also play a vital role in promoting early detection and better care. If you notice any concerning symptoms, consult a healthcare provider promptly.
💡 Note: Early diagnosis and treatment can significantly improve survival rates, with the five-year relative survival rate for ependymoma reaching 88.2%.
FAQ
What is the survival rate for ependymoma?
The five-year relative survival rate for ependymoma is approximately 88.2%. This rate depends on factors like tumor grade, location, and how early treatment begins. Early diagnosis and proper care improve outcomes significantly.
Can ependymoma recur after treatment?
Yes, ependymoma can recur, especially if the tumor is not completely removed. Regular follow-ups and imaging tests help monitor for recurrence. Your doctor may recommend additional treatments like radiation or chemotherapy if the tumor returns.
Is ependymoma hereditary?
Most ependymomas occur sporadically and are not hereditary. However, individuals with genetic conditions like neurofibromatosis type II (NF2) have a higher risk of developing spinal ependymomas. Genetic counseling may help assess your risk.
How can I differentiate ependymoma symptoms from other conditions?
Ependymoma symptoms, such as headaches, nausea, or back pain, can mimic other conditions. Persistent or worsening symptoms, especially when combined with neurological changes like seizures or weakness, warrant medical evaluation. Imaging tests like MRI can confirm the diagnosis.
Are children more affected by ependymoma than adults?
Ependymoma affects both children and adults, but the symptoms and tumor types differ. Children often experience developmental delays, irritability, or increased head size, while adults report headaches, nausea, or back pain. Early detection is crucial for both age groups.
💡 Tip: If you notice persistent symptoms, consult a healthcare provider promptly for evaluation and guidance.
See Also
Cerebellar Astrocytoma: Symptoms You Should Be Aware Of
Essential Insights Into Embryonal Carcinoma You Must Know
Choroid Plexus Carcinoma: Symptoms and Treatment Options Explained

