What Is Hepatoblastoma and Its Common Symptoms

Hepatoblastoma, a rare type of liver cancer, primarily affects children under the age of five. This condition begins in the liver and occurs when cells grow abnormally. While Hepatoblastoma isn’t commonly discussed, recognizing the signs is crucial. Early detection can significantly improve treatment outcomes. If you observe anything unusual in your child, such as a swollen abdomen or unexplained weight loss, it’s essential to consult a doctor immediately. Taking swift action could be life-saving.
Key Takeaways
Hepatoblastoma is a rare liver cancer. It mostly affects kids under five. Finding it early helps with better treatment.
Common signs are belly swelling, yellow skin, weight loss, and tiredness. See a doctor right away if you notice these.
Some genetic conditions, like Beckwith-Wiedemann syndrome, raise the risk. Familial adenomatous polyposis also increases the chance of getting it. Keep track of your child's health.
Treatments include surgery and chemotherapy. In bad cases, a liver transplant may be needed. Early diagnosis can cure over 90% of cases.
Regular doctor visits for at-risk kids can find it early. Trust your gut and get help if something seems wrong.
What Is Hepatoblastoma?
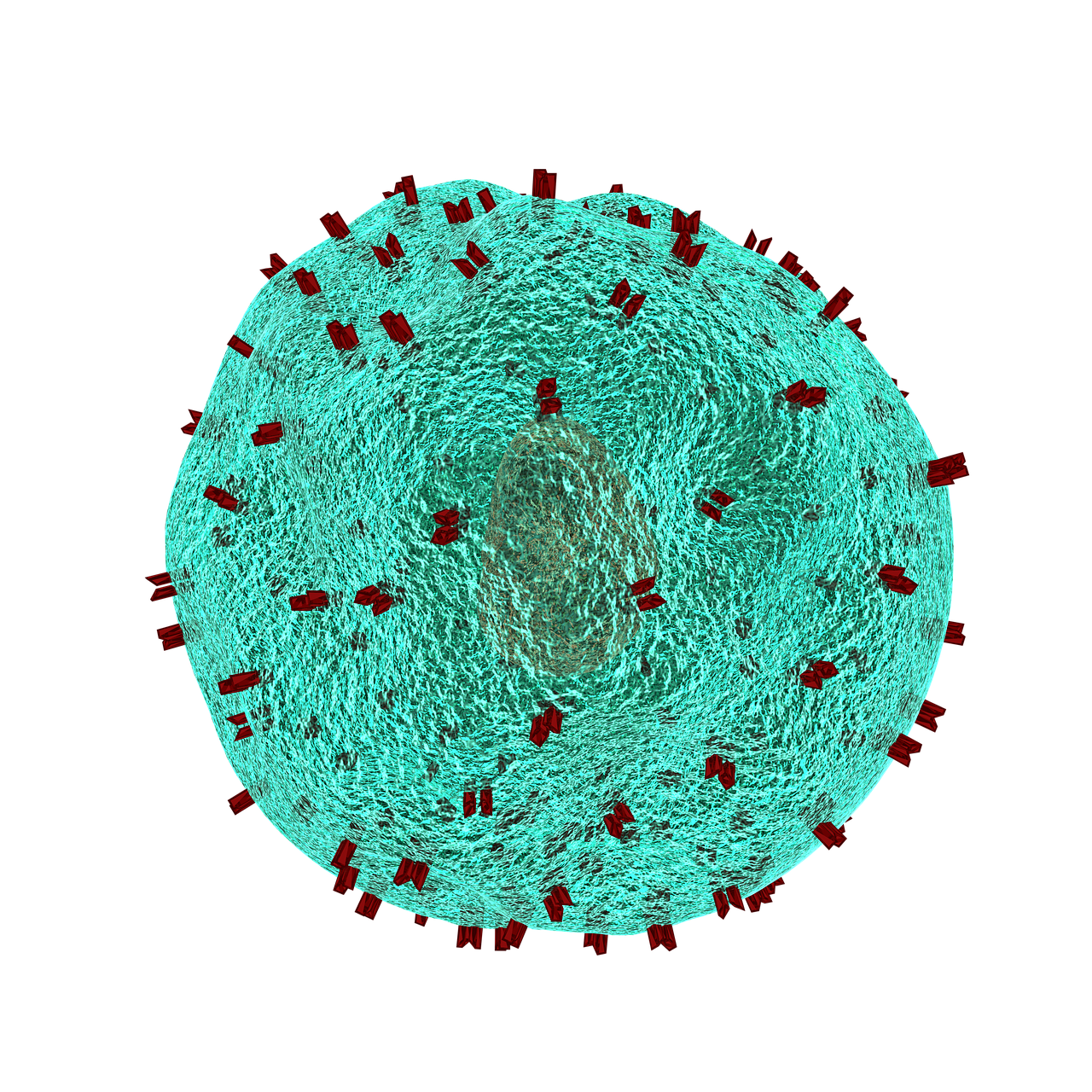
Definition and Overview
Hepatoblastoma is a type of cancer that develops in the tissues of the liver. It’s the most common liver cancer in children, especially those under three years old. Unlike hepatocellular cancer, which typically affects adults with liver conditions, hepatoblastoma occurs in young children without preexisting liver issues. This cancer starts in immature liver cells and can grow rapidly if not treated.
You might wonder how hepatoblastoma differs from other liver cancers. Here are some key points:
It usually affects one area of the liver, often the right lobe.
It can spread to other parts of the body and is classified into two types: "Epithelial Type" and "Mixed Epithelial/Mesenchymal Type."
How Common Is Hepatoblastoma?
Hepatoblastoma is rare, but it’s the most common malignant liver tumor in children. Globally, the incidence rate is about 2.3 cases per million children each year. Interestingly, the number of cases has decreased over the years, from around 6,131 cases in 2000 to 4,045 in 2021. However, studies show that the annual incidence rate increased by 4.3% between 1992 and 2004 for children under 19 years old.
Why Does Hepatoblastoma Occur?
Genetic mutations leading to abnormal liver cell growth
Hepatoblastoma often results from genetic mutations. One of the most common mutations occurs in the CTNNB1 gene, which is found in up to 80% of cases. This mutation activates the WNT signaling pathway, causing liver cells to grow uncontrollably. Mutations in the APC gene can also lead to similar effects, especially in familial cases. Additionally, variants in the NFE2L2 gene have been linked to more aggressive forms of the disease.
Association with certain genetic conditions like Beckwith-Wiedemann syndrome
Some genetic conditions increase the risk of hepatoblastoma. For example, Beckwith-Wiedemann syndrome, a disorder that causes overgrowth in various parts of the body, is strongly associated with this cancer. Children with familial adenomatous polyposis (FAP), a condition that leads to numerous polyps in the colon, are also at higher risk.
Common Symptoms of Hepatoblastoma

When it comes to hepatoblastoma, recognizing the symptoms early can make a big difference. While some signs are physical and easy to spot, others might feel more general and harder to connect to this condition. Let’s break them down so you know what to look for.
Physical Symptoms
Abdominal swelling or a noticeable lump
One of the most common signs is a swollen belly or a lump in the abdomen. You might notice your child’s stomach looking larger than usual, or you could feel a firm mass when touching their belly. This swelling happens because the tumor grows within the liver, taking up space and causing the abdomen to expand.
Pain or discomfort in the abdomen
Your child might complain about belly pain or seem uncomfortable, especially after eating. This discomfort can result from the tumor pressing against nearby organs or tissues.
Jaundice (yellowing of the skin and eyes)
Jaundice is another symptom to watch for. If your child’s skin or the whites of their eyes start turning yellow, it could mean the liver isn’t functioning properly. This happens when the tumor blocks bile flow, leading to a buildup of bilirubin in the body.
General Symptoms
Unexplained weight loss
If your child starts losing weight without any clear reason, it’s worth paying attention. A loss of appetite often accompanies this, making it harder for them to maintain their usual energy levels.
Fatigue or weakness
Feeling tired or weak is another common symptom. Your child might seem less active or struggle to keep up with their usual playtime. This could be due to the body using extra energy to fight the tumor or from anemia caused by the condition.
Fever without an apparent cause
A persistent fever with no obvious reason, like an infection, might also be a sign. It’s your body’s way of signaling that something isn’t right.
Nausea and vomiting
Nausea and vomiting can occur as the tumor grows and affects the liver’s ability to function. These symptoms might also make it harder for your child to eat or drink, leading to dehydration or further weight loss.
Tip: If you notice any of these symptoms in your child, don’t wait. Reach out to a healthcare professional for advice. Early detection of hepatoblastoma can lead to better treatment outcomes.
Risk Factors for Hepatoblastoma
Understanding the risk factors for hepatoblastoma can help you stay informed and proactive about your child’s health. While this condition is rare, certain factors can increase the likelihood of its development. Let’s explore these risks.
Age and Gender
Most common in children under 5 years old
Hepatoblastoma primarily affects young children, especially those under the age of five. This is because the liver cells in young children are still developing, making them more susceptible to abnormal growth. If your child falls within this age group, it’s important to stay vigilant for any symptoms.
Slightly more prevalent in boys
Boys are slightly more likely to develop hepatoblastoma than girls. In fact, studies show that 62.6% of diagnosed cases occur in males. Here’s a quick breakdown of the incidence rates:
Gender | Incidence per 1,000,000 |
|---|---|
Males | 1.22 |
Females | 0.96 |
While the difference isn’t drastic, it’s worth noting if you have a young son.
Genetic Conditions
Familial adenomatous polyposis (FAP)
If your family has a history of FAP, your child may face a higher risk of hepatoblastoma. FAP is a genetic condition that causes numerous polyps to form in the colon and rectum, and it’s closely linked to this type of liver cancer.
Beckwith-Wiedemann syndrome
Beckwith-Wiedemann syndrome is another genetic condition associated with hepatoblastoma. This syndrome causes overgrowth in various parts of the body and increases the likelihood of abnormal liver cell development. If your child has been diagnosed with this condition, regular check-ups with a healthcare provider are essential.
Premature Birth and Low Birth Weight
Premature birth and low birth weight (LBW) are significant risk factors for hepatoblastoma. Here’s why:
Premature infants, especially those with very low birth weight (VLBW) under 1500 grams, face a much higher risk.
Many LBW or VLBW infants receive erythropoietin during neonatal care, which may contribute to the development of this cancer.
The incidence of hepatoblastoma has doubled between 1975 and 1999, partly due to the growing number of premature births.
If your child was born prematurely or had a low birth weight, it’s a good idea to discuss these risks with your pediatrician. Early monitoring can make a big difference.
Note: While these factors may increase the risk, they don’t guarantee that hepatoblastoma will develop. Staying informed and seeking medical advice when needed can help you take the right steps for your child’s health.
Stages of Hepatoblastoma
Understanding the stages of hepatoblastoma can help you grasp how far the cancer has progressed and what treatment options might be available. Let’s break it down step by step.
Stage I: Localized tumor that can be completely removed
At Stage I, the tumor is localized, meaning it hasn’t spread beyond the liver. The good news? It can be completely removed through surgery. Doctors often perform a wedge resection or a lobectomy to take out the affected part of the liver.
Here’s a quick look at the defining characteristics of Stage I hepatoblastoma:
Characteristic | Description |
|---|---|
Resectability | Tumor is completely resectable via wedge resection or lobectomy |
Histology | Tumor has pure fetal histologic results |
AFP Level | AFP level is within reference range within 4 weeks of surgery |
For less aggressive types, like pure fetal hepatoblastoma, chemotherapy might not even be necessary. Surgery alone could be enough to treat it.
Tip: If your child is diagnosed at this stage, the chances of a full recovery are very high with timely intervention.
Stage II: Tumor mostly removed, but microscopic cancer cells remain
In Stage II, the tumor is mostly removed, but tiny cancer cells may still linger in the liver. These cells are too small to see with the naked eye but can grow if left untreated. To tackle this, doctors often recommend chemotherapy after surgery. This helps eliminate any remaining cancer cells and reduces the risk of recurrence.
Stage III: Tumor cannot be fully removed and has spread to nearby areas
Stage III is more advanced. At this stage, the tumor cannot be completely removed because it has spread to nearby tissues or lymph nodes. Surgery might still be an option, but it’s usually combined with chemotherapy to shrink the tumor and control its growth.
Note: Even at this stage, treatment options exist. Advances in medicine have made it possible to manage and treat hepatoblastoma effectively, even in more challenging cases.
Stage IV: Cancer has spread to distant parts of the body
Stage IV hepatoblastoma is the most advanced stage of this cancer. At this point, the tumor has spread beyond the liver to other parts of the body, such as the lungs, bones, or brain. This spread, known as metastasis, makes treatment more challenging. However, it’s not impossible to manage. With the right approach, many children still have a fighting chance.
Treatment for Stage IV often involves a combination of surgery, chemotherapy, and sometimes a liver transplant. Doctors aim to remove as much of the tumor as possible while using chemotherapy to target cancer cells in other areas. In some cases, a liver transplant becomes necessary if the liver is too damaged or the tumor cannot be removed entirely.
You might wonder about survival rates for children diagnosed at this stage. Here’s what you should know:
Survival rates range from 50% to 60% when surgery and chemotherapy are used together.
These rates are improving thanks to advancements in treatment, including more aggressive chemotherapy options and better access to liver transplants.
Note: While Stage IV sounds daunting, medical advancements are giving families more hope than ever before. Early and aggressive treatment can make a significant difference.
If your child is facing this diagnosis, staying informed and working closely with a medical team is crucial. Every child’s case is unique, and doctors will tailor the treatment plan to give your child the best possible outcome. Remember, you’re not alone in this journey—support and resources are available to help you navigate it.
Importance of Early Detection and Treatment
How Early Diagnosis Improves Outcomes
Catching hepatoblastoma early can make a world of difference. When diagnosed in its initial stages, treatment options are more effective, and the chances of a full recovery increase significantly. For example, children with Stage I or II hepatoblastoma often achieve cure rates exceeding 90% when treated with surgery and chemotherapy. Early detection also reduces the likelihood of the cancer spreading to other parts of the body, making treatment less invasive and more successful.
Did you know? The 5-year survival rate for children with fully resected tumors is greater than 85%. Early diagnosis plays a big role in achieving these outcomes.
Common Diagnostic Methods
Doctors use several tools to diagnose hepatoblastoma. Each method provides unique insights into the condition:
Imaging tests:
MRI is the go-to imaging test for evaluating the tumor. It helps define the tumor's margins and assess whether it can be removed surgically.
CT scans are often used to check for metastases, especially in the lungs. However, they may not be as precise as MRI for identifying residual tumors.
Abdominal radiography can reveal an enlarged liver but isn’t specific enough to confirm hepatoblastoma.
Blood tests:
Alpha-fetoprotein (AFP) testing is a key diagnostic tool. High AFP levels (greater than 500 ng/ml) strongly indicate hepatoblastoma. Doctors also monitor AFP levels during treatment to track progress.Biopsy:
A biopsy involves taking a small sample of the tumor for analysis. This step confirms the diagnosis and helps determine the best treatment plan.
Overview of Treatment Options
Once diagnosed, hepatoblastoma can be treated using a combination of methods tailored to the child’s condition.
Surgery to remove the tumor
Surgery is often the first step in treating hepatoblastoma. If the tumor is localized, doctors can remove it completely. Recent advancements in surgical techniques have improved outcomes, with survival rates for resected tumors exceeding 85%.
Chemotherapy to shrink or eliminate cancer cells
Chemotherapy is used to shrink tumors before surgery or eliminate any remaining cancer cells afterward. While effective, it can cause side effects like hearing loss or organ toxicity. Despite these challenges, chemotherapy has significantly improved survival rates, with event-free survival reaching 80% in some cases.
Liver transplant in severe cases
When the tumor is too large or located in a way that makes surgery risky, a liver transplant becomes the best option. This involves replacing the entire liver with a healthy donor organ. Liver transplants are also recommended for cases where the cancer recurs in the liver after initial treatment.
Note: Advances in treatment have made hepatoblastoma highly treatable, even in severe cases. Working closely with your child’s medical team ensures the best possible outcome.
Recognizing the symptoms of hepatoblastoma early can make a huge difference in your child’s health. Symptoms like a lump or swelling in the abdomen, unexplained weight loss, or persistent nausea shouldn’t be ignored. If you notice any of these signs, don’t hesitate to reach out to a healthcare professional.
Hepatoblastoma is treatable, especially when caught in its early stages. With advancements in medical care, many children recover fully and go on to lead healthy lives. Staying informed about risk factors, such as genetic conditions or premature birth, can also help you take proactive steps.
Your child’s health is precious. If something feels off, trust your instincts and seek medical advice promptly. Early action could save a life.
FAQ
What is the survival rate for hepatoblastoma?
The survival rate depends on the stage at diagnosis. For early stages (I and II), it’s over 85%. Even advanced stages have improved outcomes with modern treatments.
Tip: Early detection plays a huge role in improving survival rates. Always consult a doctor if you notice unusual symptoms.
Can hepatoblastoma be prevented?
Unfortunately, you can’t prevent hepatoblastoma. However, regular check-ups for children with genetic conditions or risk factors can help catch it early.
Note: If your child has a condition like Beckwith-Wiedemann syndrome, talk to your doctor about monitoring options.
Is hepatoblastoma hereditary?
Hepatoblastoma isn’t usually hereditary. However, some genetic conditions, like familial adenomatous polyposis (FAP), can increase the risk.
Condition | Risk Level |
|---|---|
Familial adenomatous polyposis (FAP) | High |
Beckwith-Wiedemann syndrome | Moderate |
How is hepatoblastoma diagnosed?
Doctors use imaging tests like MRIs, blood tests for alpha-fetoprotein (AFP), and biopsies to confirm the diagnosis.
Did you know? High AFP levels are a strong indicator of hepatoblastoma.
What are the side effects of treatment?
Common side effects include fatigue, nausea, and hair loss from chemotherapy. Surgery may cause temporary pain or discomfort.
Reminder: Always discuss potential side effects with your child’s doctor to prepare for the treatment journey.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Burkitt's Lymphoma: Key Symptoms to Recognize
Cerebellar Astrocytoma Explained: Symptoms You Should Know
Gallbladder Cancer: Symptoms and Causes You Need to Know
Endometrial Cancer Overview: Recognizing Important Symptoms
Follicular Lymphoma: Understanding Symptoms and Key Information

