What is Meningioma and What Are Its Symptoms
Meningioma is the most common type of primary brain tumor in adults, accounting for 46.1% of cases. Each year, over 170,000 people in the U.S. receive this diagnosis, which translates to approximately 97 out of every 100,000 individuals. This tumor develops in the meninges, the protective layers surrounding your brain and spinal cord. While often benign, its size and location can lead to serious health issues. You might experience symptoms like headaches, seizures, or blurred vision. In some cases, it can cause leg weakness, memory loss, or hearing problems, depending on where the tumor grows.
Key Takeaways
Meningioma is a common brain tumor in adults. It is often not cancerous but can still cause problems.
Symptoms include constant headaches, seizures, and vision problems. See a doctor if symptoms start or get worse.
Treatments include surgery, radiation, or watching the tumor. The choice depends on its size, location, and your health.
Regular check-ups are important to track health and catch the tumor if it comes back.
Knowing the tumor's type helps predict recovery. Lower types usually mean better results.
What is Meningioma?

Definition and Overview
Meningioma is a type of tumor that develops in the meninges, the protective layers surrounding your brain and spinal cord. It accounts for nearly half of all primary brain tumors in adults. Most meningiomas grow slowly and are noncancerous, but some can grow faster and invade nearby tissues. The World Health Organization (WHO) classifies meningiomas into three grades based on their growth rate and cellular characteristics. This classification helps predict how the tumor might behave and guides treatment decisions.
Types of Meningioma
Meningiomas are categorized into three main types based on their behavior and cellular features:
Characteristics | |
|---|---|
Benign (WHO grade I) | Slow-growing, less likely to invade brain, lower recurrence rate |
Atypical (WHO grade II) | Increased tissue and cell abnormalities, faster growth, higher likelihood of recurrence, often invades brain |
Malignant (WHO grade III) | Increased cellular abnormalities, fastest growth, most likely to invade brain, highest recurrence rate |
Benign Meningioma
Benign meningiomas are the most common type, representing about 80% of cases. These tumors grow slowly and usually have a distinct border, making them easier to remove surgically. They rarely invade surrounding brain tissue and have a lower chance of recurrence after treatment.
Atypical Meningioma
Atypical meningiomas account for approximately 17% of cases. These tumors grow more quickly than benign ones and often show abnormal cellular features. They may invade nearby brain tissue, making treatment more challenging. Atypical meningiomas also have a higher likelihood of coming back after treatment.
Malignant Meningioma
Malignant meningiomas, also known as anaplastic meningiomas, are rare, making up about 1.7% of cases. These tumors grow and spread rapidly, often invading surrounding tissues. They are the most aggressive type and have the highest recurrence rate, even after treatment.
Grading of Meningioma
The WHO grading system divides meningiomas into three grades based on their histological features. Each grade reflects the tumor's growth rate, invasiveness, and impact on prognosis.
Grade | Description | Prognosis Impact |
|---|---|---|
I | Benign | |
II | Atypical | Intermediate prognosis |
III | Anaplastic or Malignant | Shorter life expectancy, more aggressive |
Grade I (Low-Grade)
Grade I meningiomas are the least aggressive. They grow slowly and rarely invade nearby tissues. These tumors are easier to treat and have the best prognosis among the three grades.
Grade II (Intermediate-Grade)
Grade II meningiomas grow faster and may invade surrounding brain tissue. They often show abnormal cellular features, making them more resistant to treatment. The prognosis for these tumors is less favorable compared to Grade I.
Grade III (High-Grade)
Grade III meningiomas are the most aggressive. They grow rapidly and are more likely to recur after treatment. These tumors significantly impact life expectancy and require intensive treatment strategies.
Symptoms of Meningioma

Common Symptoms
Meningioma symptoms often develop gradually as the tumor grows. You may experience a range of symptoms depending on the tumor's size and location. Some of the most common symptoms include:
Persistent headaches
Seizures
Vision changes, such as blurriness or double vision
Nausea and vomiting
Memory problems or difficulty concentrating
Personality changes, including irritability or decreased interest in activities
Muscle weakness or numbness in specific areas of your body
Headaches are one of the earliest signs. These headaches may worsen over time or occur more frequently. Seizures, another common symptom, can vary in severity and may involve sudden muscle spasms or loss of consciousness. Vision problems, such as blurred or double vision, often occur when the tumor presses on the optic nerve.
Symptoms Based on Tumor Location
The location of the meningioma significantly influences the symptoms you might experience. Below are some examples:
Tumor Location | Symptoms |
|---|---|
Frontal Lobe | Personality changes, memory issues, leg weakness |
Temporal Lobe | Hearing loss, speech difficulties, seizures |
Spinal Cord | Muscle weakness, numbness, paralysis in limbs |
Frontal Lobe Symptoms
A tumor in the frontal lobe may cause noticeable changes in your personality or behavior. You might feel more irritable or have difficulty concentrating. Weakness in your legs is also a common symptom when the motor cortex is affected.
Temporal Lobe Symptoms
If the tumor is located in the temporal lobe, you may experience hearing loss or difficulty understanding speech. Seizures are also more likely with tumors in this area.
Spinal Cord Symptoms
Meningiomas in the spinal cord can lead to muscle weakness, numbness, or even paralysis in your arms or legs. These symptoms often worsen as the tumor grows and compresses the spinal cord.
When to Seek Medical Attention
You should seek medical attention if you notice persistent headaches, vision loss, or sudden weakness in any part of your body. New symptoms affecting your central nervous system, such as seizures or paralysis, also warrant immediate evaluation. Early diagnosis can improve treatment outcomes and prevent complications.
Risk Factors and Causes of Meningioma
Known Risk Factors
Several factors can increase your risk of developing meningiomas. Understanding these can help you identify potential concerns early.
Age and Gender
Meningiomas occur more frequently in individuals over 65 years old. Women are also at a higher risk than men, likely due to hormonal influences. However, meningiomas in men tend to be more aggressive.
Genetic Conditions
Certain genetic conditions, such as Neurofibromatosis Type 2 (NF2), significantly raise your chances of developing meningiomas. Other genetic mutations, including TRAF7, KLF4, AKT1, and SMO, may also play a role. If you have a family history of meningiomas, your risk may be higher due to inherited genetic tendencies.
Radiation Exposure
Exposure to ionizing radiation, such as from previous cancer treatments or environmental sources, is a well-known risk factor. This type of radiation can damage DNA, increasing the likelihood of tumor formation.
Other suspected factors include obesity, allergies, and even head trauma. While these associations are less clear, they may still contribute to your overall risk.
Possible Causes
Hormonal Influence
Hormones like estrogen and progesterone may influence meningioma development. These tumors are more common in women, suggesting a hormonal link. Studies have shown that elevated progesterone levels during pregnancy or from contraceptives like Depo-Provera could promote tumor growth. However, the role of estrogen remains debated, with mixed findings on its impact.
Family History
If meningiomas run in your family, you may have a genetic predisposition to develop them. Differences in DNA repair mechanisms could also play a role, making some individuals more susceptible to tumor formation.
Can Meningioma Be Prevented?
Currently, there is no guaranteed way to prevent meningiomas. However, you can reduce your risk by minimizing exposure to ionizing radiation and maintaining a healthy lifestyle. Regular check-ups and awareness of your family history can also help with early detection and management.
How is Meningioma Diagnosed?
Initial Evaluation
Diagnosing meningioma begins with a thorough evaluation by your doctor. This process typically involves several key steps:
Medical History Assessment: Your doctor will ask about your past illnesses, exposure to radiation, family history of tumors, and lifestyle habits. These details help identify potential risk factors.
Neurological Examination: You may undergo tests to check your vision, hearing, balance, coordination, strength, and reflexes. These tests help pinpoint which areas of your brain or spinal cord might be affected.
Imaging Tests: If your symptoms suggest a tumor, your doctor will recommend imaging studies to confirm its presence and location.
This initial evaluation helps your healthcare provider gather critical information to guide further diagnostic steps.
Imaging Tests
Imaging plays a vital role in diagnosing meningiomas. Two common methods are used:
MRI Scans
Magnetic Resonance Imaging (MRI) provides detailed images of your brain and spinal cord. It uses radio waves and magnets to create high-resolution pictures of soft tissues. Often, a contrast dye is injected to highlight the tumor and its boundaries. MRI is particularly effective for assessing the size, shape, and location of meningiomas. It also aids in surgical planning by offering precise neuronavigation data.
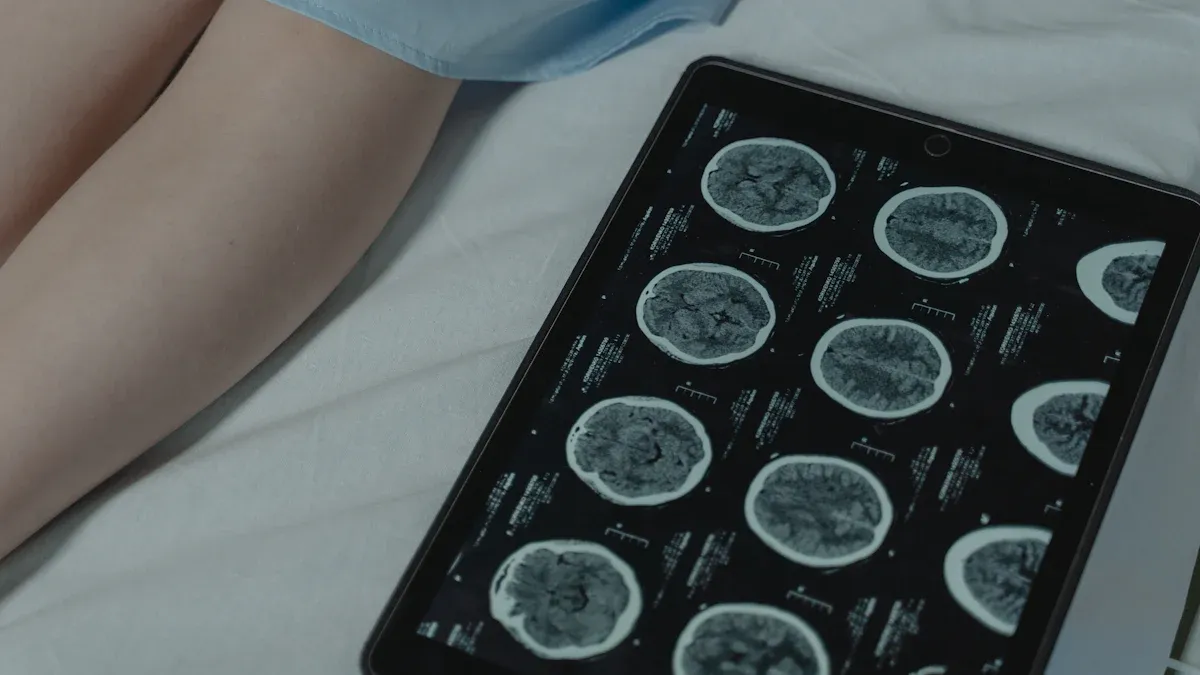
CT Scans
Computed Tomography (CT) scans combine multiple X-rays to create cross-sectional images of your brain. This method is faster and more cost-effective than MRI, making it a good option if you cannot undergo an MRI. CT scans can reveal extra-axial masses, which are often indicative of meningiomas. However, MRI is usually preferred for follow-up imaging due to its superior resolution.
Biopsy and Pathology
While imaging techniques like MRI are highly reliable, a biopsy is sometimes necessary to confirm the diagnosis and determine the tumor's grade. During this procedure, your doctor removes a small tissue sample from the tumor, often during surgery. A pathologist examines the sample under a microscope to identify cellular features and classify the tumor as benign or aggressive.
In rare cases where imaging results are inconclusive, a biopsy becomes essential. This step ensures an accurate diagnosis and helps your doctor develop the most effective treatment plan. Molecular analysis of the biopsy sample may also reveal genetic mutations that could influence your treatment options.
Early and accurate diagnosis is crucial for managing meningioma effectively. If you experience symptoms, consult your doctor promptly to begin the evaluation process.
Treatment Options for Meningioma
Observation and Monitoring
Observation may be the best approach for certain meningiomas. This strategy involves regular check-ups and imaging tests to monitor the tumor's growth. You might not need immediate treatment if the tumor is small, benign, and growing slowly. Older patients or those with poor overall health often benefit from this approach. Tumors near critical brain areas may also be observed to avoid the risks of active treatment.
Observation helps you avoid potential side effects of surgery or radiation. These treatments, while safer today, still carry risks. If your symptoms are minimal, active treatment may not improve your quality of life. Instead, monitoring allows you to maintain your daily activities without interruption.
Surgery
Surgery is often the primary treatment for meningiomas. It aims to remove as much of the tumor as possible while preserving brain function. Advances in surgical techniques have made this option safer and more effective.
Craniotomy
A craniotomy involves opening the skull to access and remove the tumor. Surgeons use tools like microscopes and neuronavigation systems to enhance precision. Neuronavigation tracks surgical instruments in real time, reducing the risk of damaging critical brain areas. This method is highly effective for larger or more complex tumors.
Minimally Invasive Techniques
Minimally invasive techniques, such as endoscopic surgery, offer an alternative to traditional craniotomy. These methods use small openings and an endoscope to access the tumor. This approach reduces recovery time and minimizes scarring. Intraoperative imaging, like MRI or CT scans, provides real-time visualization, ensuring accurate tumor removal.
Radiation Therapy
Radiation therapy is a non-invasive option for treating meningiomas. It targets tumor cells with high-energy beams, either as a standalone treatment or after surgery.
Stereotactic Radiosurgery
Stereotactic radiosurgery delivers precise radiation doses to the tumor while sparing healthy tissue. This method is ideal for small or hard-to-reach tumors. It often requires fewer sessions, making it a convenient option for many patients.
External Beam Radiation
External beam radiation uses a machine to direct radiation at the tumor. This method treats larger tumors or those in sensitive areas. It is typically delivered over several sessions to minimize side effects.
Treatment decisions depend on factors like tumor size, location, and your overall health. Consulting with your doctor ensures the best approach for your condition.
Medications and Supportive Care
Managing meningiomas often involves medications to address symptoms and complications. These drugs can improve your quality of life and support other treatments like surgery or radiation. Below is a table summarizing commonly used medications and their purposes:
Medication Type | Purpose |
|---|---|
Corticosteroids | Reduce swelling and inflammation around the tumor, especially before and after surgery. |
Antiepileptic drugs | Prevent seizures, particularly in cases where the tumor affects brain areas prone to seizures. |
Chemotherapy | Used in rare cases for malignant meningiomas when surgery and radiation are not effective. |
Corticosteroids play a critical role in reducing brain swelling, which can alleviate symptoms like headaches or nausea. Doctors often prescribe antiepileptic drugs if you experience seizures or if your tumor is located in a seizure-prone area. Chemotherapy, while less effective for most meningiomas, may be an option for aggressive or recurrent tumors. Your doctor will tailor the medication plan to your specific needs, ensuring the best possible outcome.
Supportive care also includes physical therapy, counseling, and nutritional guidance. These services help you manage side effects and maintain overall well-being during treatment. Regular follow-ups with your healthcare team ensure that your symptoms remain under control.
Factors Influencing Treatment Decisions
Several factors guide the choice of treatment for meningiomas. Understanding these can help you make informed decisions with your doctor. Below is a table highlighting key factors:
Factor | Description |
|---|---|
Tumor size and location | Larger tumors or those near critical brain areas may require more complex treatment approaches. |
Age and overall health | Younger, healthier patients often tolerate aggressive treatments better than older individuals. |
Genetic markers | Certain genetic changes may indicate a higher risk of recurrence or aggressive tumor behavior. |
Previous treatment | Recurrence after prior treatment can complicate future options and affect prognosis. |
Other considerations include life expectancy, tumor grade, and type. Lower-grade tumors generally have better outcomes, while higher-grade ones may require more intensive care. Your age and health status also play a significant role. Younger patients often recover more quickly and respond better to treatments. By discussing these factors with your doctor, you can choose a treatment plan that aligns with your goals and medical needs.
Prognosis and Survival Rates of Meningioma
Prognosis Based on Tumor Grade
The prognosis for meningioma depends largely on the tumor's grade. Tumor grade reflects its growth rate and aggressiveness, which directly impacts treatment outcomes. Here's a breakdown of how prognosis varies by grade:
Tumor Grade | Characteristics | Prognosis |
|---|---|---|
Grade I | Benign, slow-growing, well-defined borders | Generally favorable with high likelihood of complete removal and low recurrence risk |
Grade II | Atypical, intermediate aggressiveness, more rapid growth | Less favorable prognosis, increased risk of recurrence, challenging to remove |
Grade III | Anaplastic, aggressive, invasive | Poor prognosis, high recurrence risk, limited treatment response |
Other factors, such as tumor size, location, patient age, and overall health, also influence outcomes. Younger individuals with smaller, accessible tumors tend to have better prognoses. Lower-grade tumors generally lead to longer life expectancy, while higher-grade ones require more intensive treatment and carry greater risks.
Long-Term Outlook
Your long-term outlook after a meningioma diagnosis depends on several factors. Lower-grade meningiomas (Grade I) often have excellent survival rates. For example, the 5-year survival rate for noncancerous meningiomas is 96% for children under 14, 97% for individuals aged 15 to 39, and 87% for those over 40. Malignant meningiomas (Grade III), however, have a 5-year survival rate of over 67% and a 10-year survival rate of about 61%.
Factors like tumor grade, size, and location, as well as your age and overall health, play a significant role in determining survival rates. Genetic markers and previous treatments may also affect your long-term prognosis. Regular follow-ups and monitoring are essential to ensure the best possible outcomes.
Potential Complications and Recurrence
Treatment for meningiomas can lead to complications. Surgery may result in infections, bleeding, or damage to nearby brain tissues. Radiation therapy often causes fatigue, nausea, and skin irritation. Chemotherapy, though less common for meningiomas, can lead to side effects like vomiting, diarrhea, and hair loss.
Recurrence remains a concern, especially for higher-grade tumors. Incomplete tumor removal significantly increases the risk of recurrence. Certain genetic mutations may also elevate this risk. Regular imaging and follow-ups help detect any recurrence early, allowing for timely intervention.
While complications and recurrence are possible, advancements in treatment continue to improve outcomes. Staying informed and working closely with your healthcare team can help you manage these risks effectively.
Meningioma can significantly affect your health, but early detection and proper management improve outcomes. Understanding the symptoms, risk factors, and treatment options empowers you to make informed decisions.
Key takeaways include:
Surgical resection is the primary treatment for symptomatic cases.
Radiation therapy helps when complete removal isn’t possible.
Palliative care enhances quality of life during treatment.
Recovery involves regular follow-ups to monitor your health and detect recurrence. If you suspect meningioma or have concerns, consult a healthcare provider for personalized advice.
Note: Tumor classification impacts prognosis. For example:
Classification
Description
Grade I
Non-malignant, better outcomes
Grade II
Non-malignant, moderate risk
Grade III
Malignant, higher recurrence risk
FAQ
What is the most common symptom of meningioma?
Headaches are the most common symptom. They often worsen over time as the tumor grows. You might also experience other symptoms like seizures or vision problems, depending on the tumor's location.
Can meningioma go away on its own?
Meningiomas do not disappear without treatment. Some grow very slowly and may not require immediate intervention. Your doctor might recommend monitoring if the tumor is small and not causing symptoms.
Is meningioma always cancerous?
No, most meningiomas are benign (noncancerous). However, some can be atypical or malignant, meaning they grow faster and may invade nearby tissues. Your doctor will determine the tumor type through imaging and biopsy.
How long does recovery take after meningioma surgery?
Recovery time varies. Most people return to normal activities within weeks to months. Factors like tumor size, location, and your overall health affect how quickly you recover.
Can lifestyle changes reduce the risk of meningioma?
While you cannot prevent meningioma entirely, maintaining a healthy lifestyle may help. Avoid exposure to radiation, eat a balanced diet, and stay active. Regular check-ups can also aid in early detection.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Ependymoma: Key Symptoms You Should Know
Hodgkin's Lymphoma: Recognizing Its Symptoms and Signs
Cerebellar Astrocytoma: Symptoms You Need to Recognize

